Article Updated: November 14, 2023
Bed Sores and Sepsis
You can’t just look at a death certificate and conclude that a bed sore caused sepsis. This causation analysis needs some medical savvy.
I work through this analysis frequently in reviewing nursing home records, and in working with wound care consultants and geriatric specialists.
Quite often, I find that the source of the sepsis was, in fact, a negligently caused bed sore. Below, I will share some insights about this analysis.
If you still have questions after reading this article, reach out to me for help.
Clickable Table of Contents
Intro to Sepsis
1 – What is Sepsis
2 – Causes of Sepsis
Bed Sores and Sepsis Relationship
3 – Bed Sores and Sepsis Relationship
4 – Can Pressure Ulcers Cause Sepsis ?
5 – Bed Sores Sepsis & Nursing Home Victims
Bedsore Sepsis Prevention & Treatment
6 – Preventing Sepsis Open Wound Injuries
7 – Treatment of Bedsore Sepsis
Resources
8 – Bed Sores and Sepsis Legal Answers
9 – Supporting Literature, Citations & Research
10 – About the Author
11 – Legal Help in Maryland & Nationally
What is Sepsis
In its simplest form, sepsis is an infection of the blood. When a person has bed sores, sepsis can occur because chemicals are released into the body to help fight an infection.
When this happens, as with bed sores and sepsis, there can be an inflammation triggered throughout the entire system which creates a chain effect that often damages organs, causes fever, and in extreme cases, or when the infection is not caught early, can also cause death.
Symptoms of Sepsis
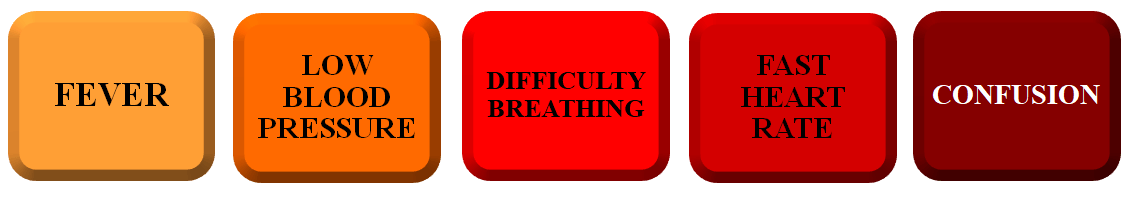
The signs of sepsis can include things seemingly benign that may come with other conditions and illnesses. However, if you have any open wounds, or have had any recent surgeries, any of the following symptoms are a potential cause for concern:
Any combination of these symptoms can be cause for concerns and should be checked out sooner than later.
Causes of Sepsis
An additional contributory cause to sepsis is the wound, or opening that was not taken care of properly, and was allowed to develop into an infection.
Bacterial infections tend to be a major cause of many sepsis infections.
Bacterial Causes
Bacterial infections are the most common cause of sepsis. While they are the most common form of sepsis infections, this does not mean they are the only kind.
Additional sources of sepsis infections are viral, fungal or even parasitic infections. Ultimately, when a foreign body enters into the blood, and there is a reaction by the body to fight it, sepsis is a potential result.
Many parts of the body can be the entry point for sepsis, the most common ones can include the abdomen, the skin and the central nervous system.
Areas Of Body Affected by Sepsis
Areas of the body that sepsis often starts from:
◊ Abdomen: Infections tend to come to the abdomen through infections in the appendix, the gallbladder and the liver.
◊ Central Nervous System: These infections tend to start from the spinal cord or the brain.
◊ Skin: Any open areas of skin, especially ones that are left untreated for a long period of time, can have bacteria enter into the system. These wounds can come from bed sores, leading to sepsis, or can also happen with poorly cared for catheters. In addition to bed sores causing sepsis, cellulitis (another skin condition) can also cause sepsis
◊ The Kidneys or Bladder: These infections usually come through the urinary tract and develop frequently with catheter use.
◊ Lungs: Conditions such as pneumonia can cause an infection to develop in the lungs.
Urinary Tract Infections & Sepsis
The urinary tract is of particular importance in conversations about bed sores and sepsis because many patients who are bedridden will need a catheter to drain urine, and these same patients are also at high risk of bed sores because they are immobile.
Infections of the kidneys or bladder can be difficult to identify, difficult to treat, and can lead to serious inflammatory responses as the body attempts to fight such infections off.
Improperly placed, and poorly cared for catheters can exasperate the potential for sepsis and make them more likely.
For those who have a catheter, and also have signs of bedsores, there is every reason to be alert and cautious that sepsis can occur, and the signs of sepsis should be watched out for diligently.
Bed Sores and Sepsis Relationship
Bed sores are very closely related to sepsis. The reason for this relationship is the frequency in which the two conditions are identified at the same time, in the same patient.
The debate around the level of strength in the relationship is disputed amongst medical professionals, with some believing that they are outright related, while others believe that the relationship is not as strong as others believe it to be.
Bed Sores and Sepsis are Related
Many in the medical community believe that a common relationship exists between bed sores and sepsis. This belief that bed sores and sepsis have a common relationship with each other stems from the high levels of sepsis seen in those who present with a bedsore.
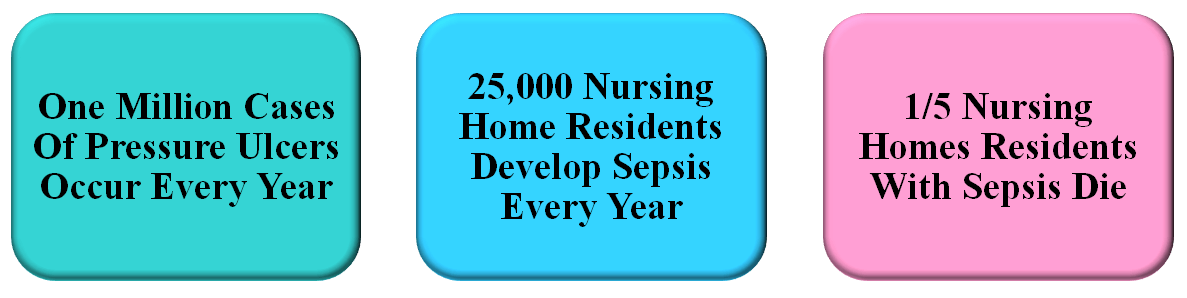
In fact, researchers have found as a very high number of sepsis cases in those who are in nursing homes or hospitals and have bed sores. Not only do many of these individuals have both bedsores and sepsis, 1/5 of them actually end up dying because their sepsis cases are so severe.
Bed Sores & Sepsis May Not Be Related
Not everyone is convinced of this however. Some researchers believe that pressure sores are not the direct cause of sepsis despite being highly related to each other in many studies.
Instead, there is the belief that other underlying medical concerns like UTIs cause sepsis more frequently when accompanied with open wounds/ ulcers and that the cause of the sepsis is the condition that caused the wound.
The belief here is that open wounds, or pressure ulcers, on their own are not a cause of sepsis. Instead, such wounds set into effect a chain reaction which ultimate leads to a patient becoming septic.
Can Pressure Ulcers Cause Sepsis ?
As noted above, the debate on this is ongoing, although it can be agreed on that open wounds, when not cared for, can lead to infections which in turn lead to the system’s inflammatory response which is sepsis.
Yes, Pressure Ulcers Can Cause Sepsis
While some believe that the pressure wounds themselves are not the case, what is known is that once the skin breaks, there is an opening that could allow bacteria to enter, causing an infection.
This is the root of sepsis. The concern within the medical and legal community is often one of semantics and order in deciding what caused what, and which medical condition can or should be blamed for the ultimate sepsis condition that patients face.
Often this means that nursing homes look for any alternate excuse for the sepsis, including preexisting conditions, compromised immune systems, recent surgeries, and a variety of other potential variables.
Because of this, industry advocates (read, nursing home puppets) believe that since bedsores and sepsis do not always go hand in hand, sepsis is nothing more than a rare outcome of pressure wounds and does not have a causal connection.
This argument is heavily focused on poking holes at the statistical relationship between a skin ulcer causing sepsis.
Bed Sores Sepsis & Nursing Home Victims
When a person develops a bed sore, it can lead to several complications, some of which can cost them their lives.
The most serious of these include sepsis because it is a serious condition that can, and often does, lead to death.
Researchers do believe that when a pressure wound is present, and there is aerobic or anaerobic bacteria present as well, the pressure ulcer is the main source of the infection.
These open sores lead to painful and deadly infections in the bones, the blood, and can cause many additional localized infections and conditions like cellulitis.
Those in nursing homes are often the victims of these conditions because they are immobile, bedridden, cannot take care of themselves and are reliant on others to give them proper medical care.
How Common Is Sepsis From Open Wounds?
Sepsis from open wounds is not the most common condition that happens in a nursing home, but there is still a much higher chance of it happening in such facilities in comparison to other settings.
Sepsis from an open wound is more common in those who are in a position where they are not getting proper care, they are not being monitored well, and their wounds are not being attended to.
Federal reports have found that sepsis was the most common reason given for people from nursing homes being transferred to hospitals and 20% of them ultimately die from their infections.
Sepsis & Probability of Death
Through careful examination of existing data on this matter, it was found that a large number of those who were in nursing homes and developed open wounds and then suffered from signs of sepsis, later died in the hospital.
Anywhere from 20% to 50% of individuals who have sepsis, can and will die from the condition.
Early medical care is needed to help control this number, but even when medical care is sought, if the individual is older or has a weakened immune system, or other medical conditions, they have a higher chance of dying from their sepsis.
Preventing Sepsis Open Wound Injuries
It comes down to infection control more than anything, as well as a close second being that sepsis is caused by open wounds which were preventable.
Weak Infection Control Practices
The most common causes of sepsis are in poor infection control in nursing homes.
Research has shown that as high as 72% of nursing homes have poor infection control programs and in some states like Illinois, this rate is as high as 88%.
Additional information given by medical doctors on the issue is that “Elderly people often don’t have the ability to bounce back from an infection” and because they are already weakened from other conditions, they cannot fight off the bedsores or the sepsis that comes with it.
If an elderly person has a bedsore, sepsis is therefore a high likelihood and dying is also a higher likelihood than in it would be in younger or healthier populations.
This is even more frightening when it is known that in the United States, approximately one million people each year may get pressure sores, and a large number of them are in nursing homes.
In sum, sepsis from open wounds is a serious condition that is not well controlled in nursing homes and has not yet been reduced nationally. This is all despite the available scientific literature highlighting the risks and relationship between sepsis and open wounds.
Treatment of Bedsore Sepsis
Treatment for bedsores are available and the best way to address a case of sepsis is to start treatment as soon as possible.
Neglect is a large part of what causes the elderly to die from sepsis and open wounds.
Even in cases that were listed as natural cause deaths, subsequent autopsies and research have found that very often neglect played a determining role in the victim’s deaths.
Fast treatment for sepsis can help avoid these deaths. The most common effective treatments for sepsis are:
◊ Antibiotics
◊ IV Treatment
◊ Wound Care
A combination of these treatments, when done as soon as possible, can help to control an infection before it starts to affect too many body parts, and can potentially save a person’s life.
Bed Sores and Sepsis Legal Answers
What if you have a death certificate or medical record that ties the sepsis to a bed sore, is your analysis done?
Absolutely not. You need to dig deeper for the causal nexus, including analysis of the particular bacteria’s present on the wound and in the blood.
I keep a separate private library with medical literature just on this one issue. I have it bookmarked, with reference to bacteria types and causal frequencies.
Long story short, I know a thing or two about bed sore sepsis malpractice, and can help you get answers.
I do hope that, either through my assistance or elsewhere, you find out what happened to your loved one and get justice against whoever did this to your family.
Warmly,
Reza Davani, Esq.
State Bar No.: #1212110211
Federal Bar No.: #30168
Cellphone: (301) 922-4598
Email: reza@nursinghometruth.com
Pressure Ulcer Legal Library
Click/Tap Icons to Access Articles

Supporting Literature, Citations & Resources:
Andersen, B. M. (2019). Prevention of Infected Pressure Sores. In Prevention and Control of Infections in Hospitals (pp. 279-285). Springer, Cham.
Wei, Z., Zhu, J., Lin, T., Cai, H., Fang, X., Zhu, Y., … & Cheng, J. (2021). Application of damage control surgery in patients with sacrococcygeal deep decubitus ulcers complicated by sepsis. Journal of International Medical Research, 49(10), 03000605211049876.
Sepsis Alliance. (2021). Sepsis and pressure ulcers: infected sores can lead to sepsis.
Fred Schulte and Elizabeth Lucas and Joe Mahr, Chicago Tribune. (2018). AVOIDABLE SEPSIS INFECTIONS SEND THOUSANDS OF SENIORS TO GRUESOME DEATHS. Healthleaders.
Christian N Kirman, MD; Chief Editor: John Geibel, MD, MSc, DSc, AGAF (2020). What is the treatment of sepsis in patients with pressure injuries (pressure ulcers)? Medscape
About the Author
This nursing home and medical malpractice article was written by Baltimore, Maryland nursing home attorney Reza Davani, Esquire. Mr. Davani received his Juris Doctor degree from a Tier 1 law school, the University of Maryland Francs King Carey School of Law. He received his first license to practice law from the State of Maryland’s Court of Appeals (MD State License No. 1212110211), and just four months later received a federal law license from the United States District Court for the District of Maryland (Federal License No. 30168).
Mr. Davani has been practicing law for over 10 years. He began practicing law by helping clients as a sanctioned student lawyer before receiving his law license, and second chaired his first jury trial in federal court before even graduating law school. He is a registered member of the Maryland Association for Justice (MAJ), the American Bar Association (ABA), the American Association for Justice (AAJ), and was formerly on the MAJ’s Legislative Leader’s Circle.
Mr. Davani has taken over 20 cases to trial in state and federal court, and favorably settled well over 100 cases for injured victims. He has personally helped his clients recover over $25,000,000 in personal injury, medical malpractice, and nursing home abuse settlements and verdicts in Maryland and other states. He is dedicated to fighting for justice, and welcomes the opportunity to help you.
About the Nurse Consultant
La kesha Dillard, started her nursing career in 1994 as a Home Health Aide (HHA). She enjoyed working with people so much that she earned her certification as a Certified Nursing Assistant (CNA). She attended Trocaire College and completed both (the LPN and RN) programs where she earned her LPN/RN AAS degree. She was motivated to further her education and in 2016 she received her baccalaureate degree in nursing from Daemen College Amherst, NY. In 2019 she successfully completed Chamberlain College of Nursing, Nurse Executive and Leadership program, and earned a Masters of Science in Nursing (MSN) degree.
Mrs. Dillard wanted to learn more about the business side of nursing, so she attended Devry University and received her Master of Business Administration (MBA) degree in 2023.
In 2021, she successfully completed the Vicky Millazo program where she earned her certification as a Legal Nurse consultant. She opened up her nurse consulting business in 2022 and is the proud owner, founder/CEO at Mrs. RN Consulting, LLC. La kesha has consulted and worked with many attorneys by helping them understand the medical records to get justice for their clients. She has worked at several Long-Term Care facilities (LTC), medical surge units and has several years of experience with patient care and consulting.
She is a strong advocate for patients and believes in Person-Centered Care (PCC) at all times. La kesha is also a tough upholder for staff rights, and she continues to motivate nurse entrepreneurs to further their education in nursing.
Bed Sores & Sepsis Malpractice Lawyer Near You in Baltimore, Maryland, Helping Clients Nationally
I can help you anywhere in Maryland, including Allegany County, Anne Arundel County, Baltimore City, Baltimore County, Carroll County, Calvert County, Caroline County, Cecil County, Charles County, Dorchester County, Frederick County, Garrett County, Harford County, Howard County, Kent County, Montgomery County, Prince George’s County, Queen Anne’s County, Somerset County, St. Mary’s County, Talbot County, Washington County, Wicomico County, and Worcester County.
I have helped clients in over a dozen jurisdictions, including California, Delaware, District of Columbia, Georgia, Illinois, Iowa, Massachusetts, Maryland, Mississippi, New Jersey, New Mexico, New York, North Carolina, Pennsylvania, South Carolina, Washington, and Virginia.
I help injured victims nationwide in all 50 states on a case-by-case basis via Pro Hac Vice.