Article Updated: November 14, 2023
Deep Tissue Injury on Heel
Deep tissue injuries develop on heels because it’s one of the common pressure points for bed bound patients. That is common because most bed bound patients spend substantial time on their back.
Thankfully, these heel DTIs are easy to spot (because the foot is typically exposed) and also easy to treat with low cost interventions.
Due to that, however, it raises the question – if such avoidance is so easy, why did I or my family member get a deep tissue injury on their heel?
The simple answer is medical negligence. With my medical malpractice insights, I dig into this issue for you in the educational article below.
Clickable Table of Contents
Deep Tissue Injury Heel
1 – Deep Tissue Injury on Heel Defined
2 – Deep Tissue Heel Injury Causes
3 – DTI & Purple Heel
4 – DTI Heel Treatments
5 – Deep Tissue Injury To The Heel Q&A
6 – Heel DTI Legal Inquiries
Resources
7 – Supporting Literature, Citations & Research
8 – About the Author
9 – Legal Help in Maryland & Nationally
Deep Tissue Injury on Heel Defined
Deep tissue injuries (DTI) come as a result of pressure on parts of the body that are pressed against a surface for a long period of time. This tends to happen often in elderly patients in nursing care, or individuals who are recovering from a medical procedure and are in a bed for an extended period of time.
When there is pressure most often it is on heels of the foot which leads to a high number of DTIs on the heel.
Early signs exist of a DTI on the heel can be seen with the presence of a skin rash caused by inflamed blood capillaries which present as a rash. This rash is indicative of a disruption in the flow of blood to an area of skin.
This kind of pressure on the tissue eventually can spread to the bony area of the heel as well which leads to hypoxic injury and tissue death.
The level of death in tissue seen with heel DTI is similar to when an individual has been dead for 45 minutes. The reason for this is that deep tissue injury to the heel causes ischemia.
Ischemia is a condition where oxygen and blood flow are restricted to an area of the body which leads to the tissue in the area starting to die.
Prevalence of DTI In The Heel
Deep tissue injury to heels is accompanied with ischemia and the high pressure to the bottom of the foot from being in a laying down position starts with a heel that is purple or has a ‘bruised’ look to them.
Deep tissue injury to the heels is common in the long term care setting and data suggest that heels are the second most common site for a DTI after the sacrum.
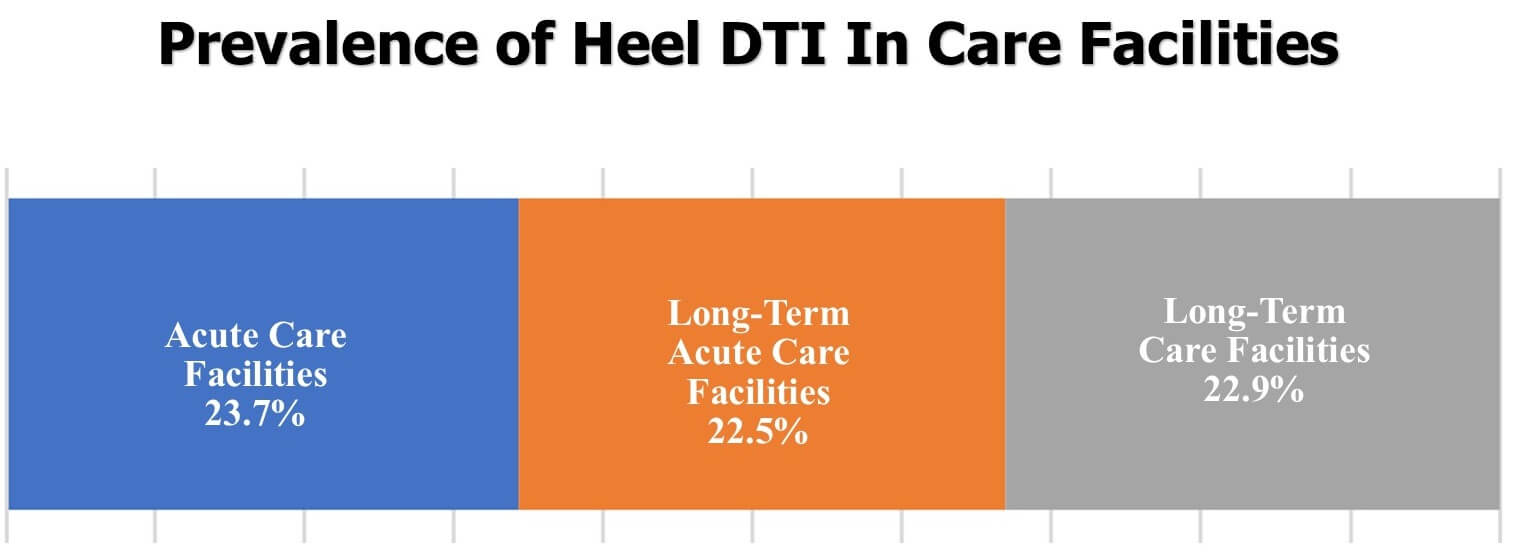
In acute care facilities, heel DTIs account for almost 24% of all cases of DTIs, 22.5% in long-term care facilities and overall 41% of all DTIs occur in the heels.
Deep Tissue Heel Injury Causes
Deep tissue injury to the heel comes when layers of deep muscle that cover bony prominences become exposed to pressure and stress when prolonged compression creates increased stiffness around the tissue and bone areas. When this happens, the skin is more prone to ischemia and tissue death.
Deep tissue injuries are not easy to diagnose because the majority of cases start with injuries deep inside the foot which cannot be seen on the surface. Most heel ulcers develop from the same commonly identified factors:
◊ Pathomechanics
◊ Chronic hypoxia/reperfusion injury
◊ Impaired nutrient supply
◊ Growth factor abnormalities
◊ Chronic inflammation
DTIs overall are most often associated with prolonged pressure to the skin and soft tissue around the heels which leads to pain and agitation in the feet.
Another major cause of deep tissue injury to heels comes from the use of devices that restrict a patient’s movements. Devices that do this include casts, tractions boots and abduction pillows which leads to lowered mobility in the feet.
Any device that restricts blood flow and also makes it harder to inspect the heel and foot can lead to deep tissue injuries to the heels.
Surgeries that limit mobility can also lead to higher DTI in the heels. In hop fracture surgery patients for example, heel ulcers are reported in 66% of patients.
DTI & Purple Heel
Purple heel is often associated with deep tissue injury to the heels. Change in color to the heel is a sign of impending or evolving DTI. Purple heel shares many things in common with DTI and often happens alongside DTIs.

Different colors on the heel in general do mean specific conditions may be occurring within the deeper tissue layers of an individual.
Some examples of this are:
◊ Red discoloration: hyperemia and ischemia
◊ Purple Discoloration: infarction
◊ Black Discoloration: necrosis
All of these are part of the deep tissue injuries that can occur on the heel commonly and lead to serious medical conditions, diminished life and the need for long-term medical care.
DTI Heel Treatments
Prevention of deep tissue injury to the heel requires there to be proactive measures taken to ensure that a DTI is prevented. Daily skin assessments in people who are prone to DTIs are one of the best treatment courses because this allows there to be identification of the silent symptoms that indicate a DTI is forming.
While prevention is the best course of action for a DTI, this is not always possible, and reactive treatments are needed. Limb compression is one of the treatments that have been shown to assist with deep tissue injuries to the heel.
An approach for this is called intermittent pneumatic compression (IPC) which has been shown to be “well tolerated by patients and provides benefits that may not be achieved using sustained compression”.
Treatments are limited because DTIs are a difficult group of lower extremity wounds to manage and treat successfully unless they are identified very early on.
Liability exists with these cases because there can be a variety of underlying health issues within the patient as well as a multitude of reasons that the DTI in the heel developed due to negligent medical care.
Mobility and the setting of care can also help with treatment viability. When treatment is at its best, there can be DTI recovery that happens without tissue loss.
Deep Tissue Injury To The Heel Q&A
How is a deep tissue injury to the heel treated?
Treatment for a DTI is mainly focused on prevention where there are daily checks of the skin and the person is moved frequently. In addition to those, compression of the heel and treatment of underlying medical conditions are also used to treat a DTI.
Are DTIs in the heel common?
Yes, DTIs in the heel are very common and for those in long-term care, or those who have recently had surgery and are bedridden, there is a very high chance that a person will develop DTI in the heel.
Can deep tissue injury related to the heel be prevented?
Yes, in fact, prevention is the best way to deal with a DTI in the heel. Ensuring that a person is mobile, hydrated and having their underlying issues dealt with are the best way to help ensure that DTI in the heel either is prevented, or treated very early on before the condition gets worse.
What affects a medical claim in a DTI case?
A medical claim for a DTI case will most be affected by the level of care that the person received leading to the discovery of the DTI as well as what steps were taken to treat the DTI.
Why is the heel so frequently affected with a DTI?
The heel is often affected by a DTI because of the level of pressure that is put on the heel on a consistent basis. When the pressure gets to be too much, particularly after any kind of surgery or during any type of recovery process, the heel tends to suffer a loss of blood flow and oxygen from constant pressure.
Heel DTI Legal Inquiries
I receive may calls from injured patients who suffered or are suffering from a DTI. This is one of those injuries that is likely the result of medical negligence, but that does not provide you a sufficient recovery to justify pursuing via a medical malpractice case which is likely to cost tens of thousands of dollars.
If you have a deep tissue injury on your heel, you need to document, document, document, as much as possible. That way, if the injury progresses (say, for example, to an open pressure wound), you will have evidence that will help hold the negligent medical providers accountable.
Warmly,
Reza Davani, Esq.
State Bar No.: #1212110211
Federal Bar No.: #30168
Cellphone: (301) 922-4598
Email: reza@nursinghometruth.com
Pressure Ulcer Legal Library
Click/Tap Icons to Access Articles

Supporting Literature, Citations & Resources:
ICD-10-CM Deep Tissue Pressure Injury will no longer be coded as an Unstageable Pressure Ulcer.
Gregory Thompson MD – Internal Medicine& Adam Husney MD – Family Medicine& Kathleen Romito MD – Family Medicine & Margaret Doucette DO – Physical Medicine and Rehabilitation, Wound Care, Hyperbaric Medicine. (2021). Pressure Injuries: Stages
Bell, D. (2019). Pertinent Principles In Healing Heel Ulcers. Podiatry Today.
Salcido R, Lee A, Ahn C. Heel pressure ulcers: purple heel and deep tissue injury. Adv Skin Wound Care. 2011 Aug;24(8):374-80; quiz 381-2. doi: 10.1097/01.ASW.0000403250.85131.b9. PMID: 21768788.
Salcido, Richard MD; Lee, Augustine MD; Ahn, Chulhyun MD, MS Heel Pressure Ulcers, Advances in Skin & Wound Care: August 2011 – Volume 24 – Issue 8 – p 374-380 doi: 10.1097/01.ASW.0000403250.85131.b9
Cynthia A Fleck, MBA, BSN, RN, FACCWS President. (2007). “Suspected Deep Tissue Injury”. American Academy of Wound Management (AAWM).
Trudie Young, Paul Chadwick, Jacqui Fletcher, Brenda King, Alison Schofield, Karen Staines, Kathryn Vowden, Michael Clark (2021). The benefits of intermittent pneumatic Compression and how to use Wound-Express in practice.
Montoya, L. (2021). Pressure Injuries, Deep Tissue Pressure Injury (DTPI). Wound Source.
Black, J., PHD Treating heel pressure ulcers, Nursing2005: January 2005 – Volume 35 – Issue 1 – p 68
About the Author
This nursing home and medical malpractice article was written by Baltimore, Maryland nursing home attorney Reza Davani, Esquire. Mr. Davani received his Juris Doctor degree from a Tier 1 law school, the University of Maryland Francs King Carey School of Law. He received his first license to practice law from the State of Maryland’s Court of Appeals (MD State License No. 1212110211), and just four months later received a federal law license from the United States District Court for the District of Maryland (Federal License No. 30168).
Mr. Davani has been practicing law for over 10 years. He began practicing law by helping clients as a sanctioned student lawyer before receiving his law license, and second chaired his first jury trial in federal court before even graduating law school. He is a registered member of the Maryland Association for Justice (MAJ), the American Bar Association (ABA), the American Association for Justice (AAJ), and was formerly on the MAJ’s Legislative Leader’s Circle.
Mr. Davani has taken over 20 cases to trial in state and federal court, and favorably settled well over 100 cases for injured victims. He has personally helped his clients recover over $25,000,000 in personal injury, medical malpractice, and nursing home abuse settlements and verdicts in Maryland and other states. He is dedicated to fighting for justice, and welcomes the opportunity to help you.
About the Nurse Consultant
La kesha Dillard, started her nursing career in 1994 as a Home Health Aide (HHA). She enjoyed working with people so much that she earned her certification as a Certified Nursing Assistant (CNA). She attended Trocaire College and completed both (the LPN and RN) programs where she earned her LPN/RN AAS degree. She was motivated to further her education and in 2016 she received her baccalaureate degree in nursing from Daemen College Amherst, NY. In 2019 she successfully completed Chamberlain College of Nursing, Nurse Executive and Leadership program, and earned a Masters of Science in Nursing (MSN) degree.
Mrs. Dillard wanted to learn more about the business side of nursing, so she attended Devry University and received her Master of Business Administration (MBA) degree in 2023.
In 2021, she successfully completed the Vicky Millazo program where she earned her certification as a Legal Nurse consultant. She opened up her nurse consulting business in 2022 and is the proud owner, founder/CEO at Mrs. RN Consulting, LLC. La kesha has consulted and worked with many attorneys by helping them understand the medical records to get justice for their clients. She has worked at several Long-Term Care facilities (LTC), medical surge units and has several years of experience with patient care and consulting.
She is a strong advocate for patients and believes in Person-Centered Care (PCC) at all times. La kesha is also a tough upholder for staff rights, and she continues to motivate nurse entrepreneurs to further their education in nursing.
Deep Tissue Injury Lawyer Near You in Baltimore, Maryland & Beyond
I can help you anywhere in Maryland, including Allegany County, Anne Arundel County, Baltimore City, Baltimore County, Carroll County, Calvert County, Caroline County, Cecil County, Charles County, Dorchester County, Frederick County, Garrett County, Harford County, Howard County, Kent County, Montgomery County, Prince George’s County, Queen Anne’s County, Somerset County, St. Mary’s County, Talbot County, Washington County, Wicomico County, and Worcester County.
I have helped clients in over a dozen jurisdictions, including California, Delaware, District of Columbia, Georgia, Illinois, Iowa, Massachusetts, Maryland, Mississippi, New Jersey, New Mexico, New York, North Carolina, Pennsylvania, South Carolina, Washington, and Virginia.
I help injured victims nationwide in all 50 states on a case-by-case basis via Pro Hac Vice.