Article Updated: November 14, 2023
How Often Should Bed Bound Residents Be Repositioned
It’s really not that difficult – if nursing homes and hospitals are doing their job (i.e., following the “standards of care”), they will:
◊ Plant for a patient/resident’s lack of mobility
◊ Implement interventions (such as turning and repositioning schedules)
◊ Monitor those plans and interventions to make they’re being followed
I have reviewed well over 100 patient/resident charts where a key issue was repositioning. I have seen negligence. I have seen fraud. I have seen injustice, with avoidable injuries caused by medical negligence.
In this article, you will benefit from my decade of personal injury experience as I deep dive into the million dollar issue for all pressure wound cases – resident repositioning.
Clickable Table of Contents
Patient Repositioning Basics
1 – Patient Repositioning Importance
2 – Assistance with Repositioning by Nurses
3 – How Often Should You Reposition a Patient?
Patient Repositioning Safety
4 – Turning Patients Every 2 Hours: Benefits
5 – 2 Hourly Repositioning: Doctors Agree
6 – 2 Hourly Repositioning: Scientists Agree
Tools to Help Bed Bound Residents be Repositioned
7 – Turning And Repositioning Chart
8 – Turning Schedule Printouts
9 – Other Turning And Repositioning Tools
Resources
10 – Help if Bed Bound Residents Were Not Repositioned
11 – Supporting Literature, Citations & Research
12 – About the Author
13 – Legal Help in Maryland & Nationally
Patient Repositioning Importance
People who have been in the hospital, are in a nursing home or are limited to laying down in one position for an extended period of time will have a higher chance of sores on their body. These sores are serious and can cause infection, loss of limbs and even death.
You may believe that a condition so serious must be difficult to treat but this is not the case. In reality, these kinds of sores have one simple solution that can help to mitigate them from occurring, and that is patient repositioning.
A person who is forced to sit or lay down for a long period of time cannot move on their own often and will need assistance with repositioning. A nurse or assisted living care staff can help and be that assistance.
The question is how often should a bedridden patient be turned?
The answer to this has been given by doctors, nurses and scientists alike, all of who have made clear that turning patients every 2 hours is an ideal way to mitigate sores from developing.
Assistance with Repositioning by Nurses
Patient repositioning is a well-known policy in nursing homes and hospitals. Since the question of how often should a bedridden patient be turned has been answered, the major focus of nursing homes should be to offer assistance with repositioning.
Turning patients every 2 hours is a policy that additionally is enshrined into federal safety standards as a necessary common practice that is not a suggestion, but rather a rule to abide by.
It is the task of nurses and care providers to ensure that patients are turned every 2 hours no matter how busy their schedules get.
While constraints on nursing time are a serious concern, at the end of the day, failure to reposition leads to sores and nursing staff are responsible for daily care that helps to prevent this.
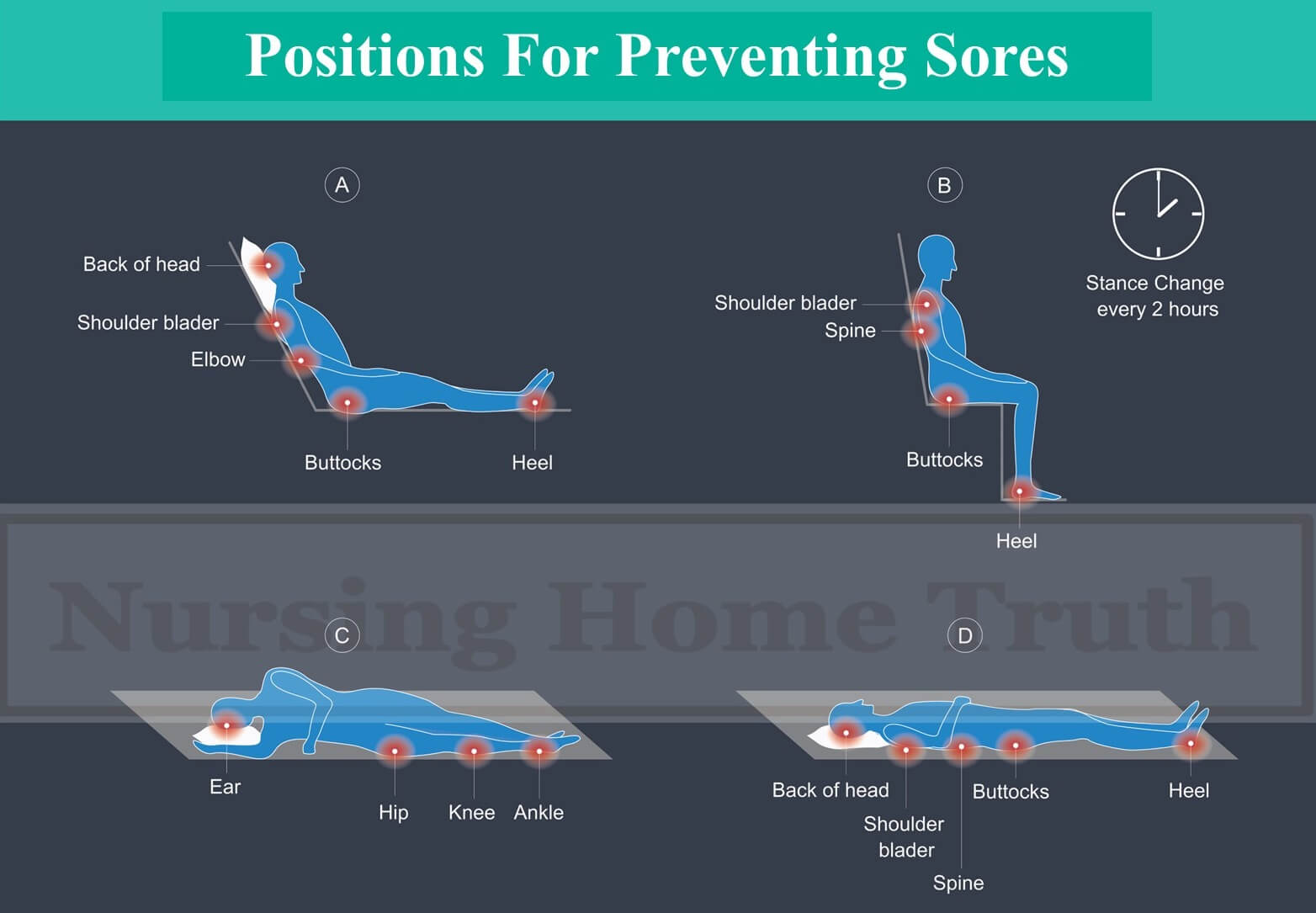
Many different positions can be used by nursing staff including using a 30° tilt and the more standard 90° position, as well as laying down on the back or the sides, all of which have support as a form of preventative treatment for sores.
There is no question of whether or not 2 hour repositioning or nursing playing a role are needed or important as both have been shown to be the case.
The problem with nursing homes and repositioning are that far too many nurses fail to adequately follow clinical guidelines because of poor training or lack of adequate staffing.
How Often Should You Reposition a Patient?
Generally Accepted Standard
Patient repositioning should be done every 2 hours when a person is laying down.
There is a change in how often a bedridden patient should be turned when the person is sitting. For example if spending substantial time in a wheelchair, the resident should be repositioned every 1 hour.
In either case, the individual will likely need assistance with their repositioning which will mean a nurse or care worker will need to be there to ensure this is done.
How Following the Standard Helps Avoid Injury
Turning a patient every 2 hours is the best course of action for prevention of sores because the cause of the sores comes from stress or weight on body parts for too long a period of time. When the pressure is not relieved periodically the skin and flesh begins to break down.
Even though it has been shown that turning patients every 2 hours is the key to preventing such sores, many nurses are failing in providing this needed rotation.
Some of the early nursing interventions should be turning the patient every 2 hours, cushioning, preventing moist and inspecting the patient’s body daily.
Data on the Problem
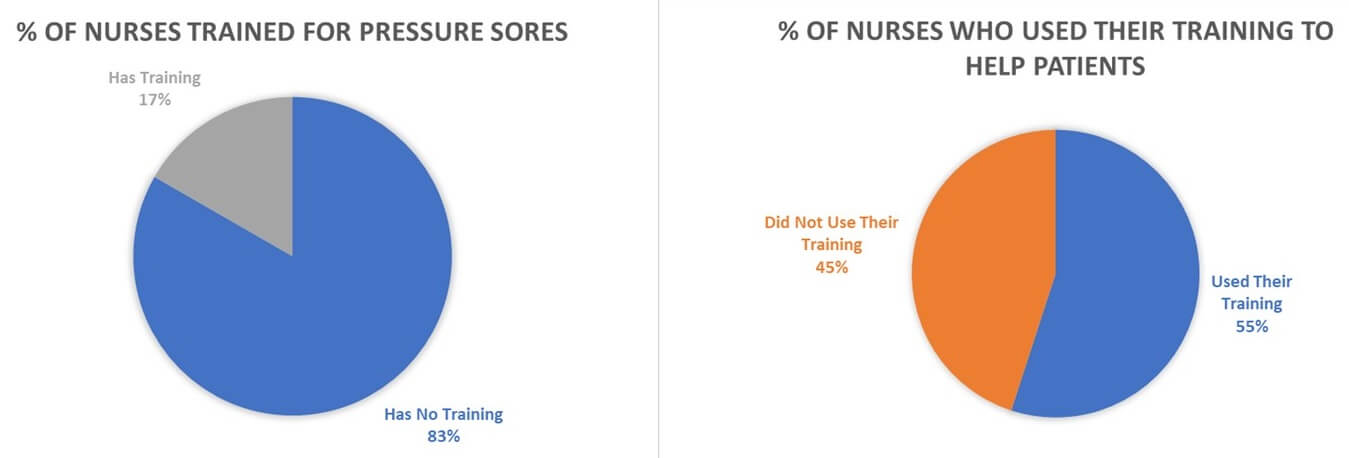
One study of hundreds of nurses found that nurses in hospital settings were not consistently providing preventative care for ulcers of this kind.
Nurses are found to have on average minimal training on sores and even those who did receive training 45% do not even use that training when treating patients.
Repositioning a patient every 2 hours is a needed and vital part of care that patients receive in nursing homes and hospitals. Despite this kind of care being known as the best course of action, only 13% of nurses evaluate their own patient care in this area as being adequate.
Turning Patients Every 2 Hours: Benefits
Patient repositioning has many benefits for those who are bedridden or forced to sit in a chair for a long period of time. Those who cannot move freely on their own or need assistance with repositioning benefit greatly when every 2 hours they are repositioned.
By turning a patient every 2 hours, many serious medical conditions can be discovered and a patient’s life can be saved as stage 3-4 sores on the body often lead to blood poisoning and even death.
Mitigate Overheating of the Body
One effect on the body of being in the same position for an extended period of time is that it overheats. When a person lies in the same position for an extended period of time the bed overheats and their body also overheats.
This kind of overheating causes sores on the body because one part of the body is constantly being exposed to weight and heat. Heat, in turn, can lead to moisture, which is a catalyst for bed sores.
Sores from the bed can be avoided when overheating is avoided and overheating can be mitigated through repositioning of the body every 2 hours.
Improve Circulation & Recovery
Turning patients every 2 hours helps with circulation in the body which in turn helps to avoid the onset of major health problems like clotting and compromised skin.
An individual who is not getting enough movement develops potential for blood pressure concerns, stiffening of joints, increased risk of clotting and increased risk of degradation to the skin.
All of this not only causes new health problems, but it also slows down recovery for existing health conditions.
While repositioning the body every 2 hours is not a solution to all health problems for a bed bound resident, it can majorly mitigate many of the problems that are associated with being bedridden for too long; namely, pressure wounds.
Avoid Serious Illnesses
Being moved frequently also means that an individual can be spared many serious illnesses that come from being in one position for too long.
Being bedridden for an extended period can lead to infections on the skin, deep in the flesh and even into the bones.
When not treated, these same infections can lead to poisoning of the blood, long-term hospitalization, intense pain and even death in serious cases.
Prevent Sores
One of the outcomes of being bedridden for an extended period of time is the potential for sores on the skin to develop. These sores can become infected and very quickly degrade the skin, flesh and bone in the affected area.
Preventing these sores is an imperative part of hospital and nursing home care. Without repositioning of the body every 2 hours, the chances that a sore will develop on the body increases and with that increase comes the potential for serious medical conditions.
Preventing sores in people who are bedridden therefore goes hand in hand with repositioning a person every 1-2 hours.
2 Hourly Repositioning: Doctors Agree
Doctors agree that a turning schedule in which 2 hourly repositioning is followed is the best course of action for bedridden patients.
One of the Earliest Interventions
Patient repositioning has been stated as one of the earliest interventions for preventing sores on the body.
Not only sores, doctors and clinicians have stated that patient repositioning can help avoid complications like “cellulitis, bone and joint infection [and some forms of] cancer” which all come when a bedridden patient is not given assistance with repositioning.
A Very Quickly Developing Problem
When asked how often should bed bound residents be repositioned, doctors tend to believe that the more the patient is moved, the better it is for their health.
Physicians and researchers have stated that a pressure wound can develop in as little as “4-6 hours with some developing in as little as just 1 hour of exposure”.
Knowing this medical information regarding pressure wound onset and etiology, it becomes obvious why a resident should be repositioined at an interval that falls well below that 4 hour mark; hence, 2 hour repositioning.
2 Hourly Repositioning: Scientists Agree
It is not only doctors who believe that patient repositioning is important but also scientists who think that a turning schedule is needed for bedridden patients.
Patients who are bedridden need assistance with 2 hourly repositioning because without this help they risk serious medical conditions. Researchers have made clear how often a bed bound resident should be repositioned and it mirrors what doctors say.
Reduce Continuous Pressure
In order to prevent a pressure ulcer it is important to reposition a patient in regular intervals. Reducing continuous pressure is difficult and not always possible when caregivers are not available.
Because of this difficulty, scientists and researchers have developed new technology to reduce the pressure on specific spots of the body. One such tool can be seen in smart air mattresses that control pressure on specific spots of the body.
The driving force behind this invention and others like it have been from the belief by scientists that constant movement helps to reduce pressure on the body.
Turning Schedules Are Important
Turning the body is not easy when there are limited resources to help with physical movement of the body. Not all individuals, hospitals or nursing homes will have access to costly air mattresses and instead have to rely on traditional methods of moving bedridden patients.
One way scientists and doctors have responded to this is through the creation of and promotion of patient turning schedules.
These schedules are created to help make sure that all patients are able to be moved at least every 2 hours so that sores on the body can be avoided.
Turning And Repositioning Chart
A turning schedule is a common and important aspect of preventing sores on those who are bedridden. Turning and repositioning charts are one of the most cost effective and useful tools nursing homes and hospitals have to make sure that 2-hourly repositioning is adhered to as much as possible.
Caretakers in busy nursing homes often have to ask how often should you reposition a patient and when was the last time a patient was moved.
A chart is often the answer to both of these questions. This is a chart that simply helps to retain a careful schedule and track how often a patient has been seen and at what intervals the patient has already been moved.
If a provider is unsure as to how often they should turn a bed bound patient, they can simply refer to the patient’s chart to see when they were last repositioned to ensure they have not been left unmoved for too long.
Turning Schedule Printouts
There is no singular turning schedule printout but there are common pieces of information in such printouts.
Turning schedule printouts track information like the patient’s name, how long they have been in one position, when they were last moved, and the exact side of the body they have been laying on.
Reposition schedules list an entire 24-hour schedule and blank spots can easily be seen visually along with signatures for who last saw the patient.
In their simplest form, these printouts ensure that there is accountability and fewer mistakes in repositioning of the patient.
Other Turning And Repositioning Tools
Charts are the most accessible and simple manner to ensure that 2-hour repositioning is taking place properly. However, other tools can also be used to help ensure that sores are avoided with patients who are bedridden.
A call light system has been used in some nursing practice to help create an alert system that acts like a digital turning schedule for nurses to help ensure that they do not forget to turn a patient for too long.
Systems like this help to avoid confusion when looking into how often you should turn a bed bound patient.
Other alert systems have also been created like the Bedsore Easing System which uses both a hardware system and a software system to alert to the problems of repositioning using a database. This system uses a Pocket Device Unit (PDU) which is assigned to a nurse with an alarm system to help them remember to reposition the patient.
Help if Bed Bound Residents Were Not Repositioned
If you or a family member has a bed wound, and you are reading this article, it is because you already know the million dollar question and it concerns repositioning.
Based on scientific literature, medical literature, and federal publications I have researched on this issue, there is a 95%+ likelihood that the wound in question was preventable and avoidable. That means that the wound exists because preventative steps were not taken; i.e., proper repositioning.
The medical chart does not speak for itself. I have seen many instances of bad charting and fraud to hide that nurses were not repositioning a resident.
You need to evaluate the turning and repositioning records, nutritional logs, medical orders, care plans, and more, to get a comprehensive view of whether the medical facility did what it was supposed to do.
I do this for a living, with a honed focus on nursing home and hospital bed sores. Point in fact, I have a private library of medical literature on this topic, and have connections with over a dozen wound care certified nurses who investigate these issues for me.
If you have suspicions that a friend or family is being neglected by a medical facility, call me for immediate help. If you don’t call me, call any competent nursing home lawyer who specializes in pressure wound claims. In the end, I hope you get answers and justice for what was, and is, being done to you.
Warmly,
Reza Davani, Esq.
State Bar No.: #1212110211
Federal Bar No.: #30168
Cellphone: (301) 922-4598
Email: reza@nursinghometruth.com
Pressure Ulcer Legal Library
Click/Tap Icons to Access Articles

Supporting Literature, Citations & Resources:
Jaichandar, K. S., & García, E. A. M. (2011, December). Intelli-sense bed patient movement sensing and anti-sweating system for bed sore prevention in a clinical environment. In 2011 8th International Conference on Information, Communications & Signal Processing (pp. 1-5). IEEE.
Saleh, B. S., Nusair, H., Al Zubadi, N., Al Shloul, S., & Saleh, U. (2011). Retracted: The nursing rounds system: Effect of patient’s call light use, bed sores, fall and satisfaction level. International Journal of Nursing Practice, 17(3), 299-303.
Salcido, R. (2004). Patient turning schedules: why and how often? Journal of Advances in Skin and Wound care. PubMed 17(4), 156.
Rivas, K. (2021). What Are Bedsores and How to Heal Them. Medihealth
Leaticia, K. S. B., Ismael, D. K., & Kombou, V. (2019). Knowledge and Contribution of Nurses in the Prevention of Bedsore Decubitus in the Surgical Ward. Available at SSRN 3723222.
Kommey, B. (2021). A Smart System to Ease Occurrence of Bedsores. Journal of Electronics, Electromedical Engineering, and Medical Informatics, 3(3), 156-163.
Nair, P., Mathur, S., Bhandare, R., & Narayanan, G. (2020, July). Bed sore Prevention using Pneumatic controls. In 2020 IEEE International Conference on Electronics, Computing and Communication Technologies (CONECCT) (pp. 1-5). IEEE.
Özdemir, H., & Karadag, A. (2008). Prevention of pressure ulcers: a descriptive study in 3 intensive care units in Turkey. Journal of Wound Ostomy & Continence Nursing, 35(3), 293-300.
Network, C. N. C. (2016). Repositioning for pressure ulcer prevention in adults—A Cochrane review. International journal of nursing practice, 22, 108-109.
Ody‐Brasier, A., & Sharkey, A. (2019). Under pressure: Reputation, ratings, and inaccurate self‐reporting in the nursing home industry. Strategic Management Journal, 40(10), 1517-1544.
About the Author
This nursing home and medical malpractice article was written by Baltimore, Maryland nursing home attorney Reza Davani, Esquire. Mr. Davani received his Juris Doctor degree from a Tier 1 law school, the University of Maryland Francs King Carey School of Law. He received his first license to practice law from the State of Maryland’s Court of Appeals (MD State License No. 1212110211), and just four months later received a federal law license from the United States District Court for the District of Maryland (Federal License No. 30168).
Mr. Davani has been practicing law for over 10 years. He began practicing law by helping clients as a sanctioned student lawyer before receiving his law license, and second chaired his first jury trial in federal court before even graduating law school. He is a registered member of the Maryland Association for Justice (MAJ), the American Bar Association (ABA), the American Association for Justice (AAJ), and was formerly on the MAJ’s Legislative Leader’s Circle.
Mr. Davani has taken over 20 cases to trial in state and federal court, and favorably settled well over 100 cases for injured victims. He has personally helped his clients recover over $25,000,000 in personal injury, medical malpractice, and nursing home abuse settlements and verdicts in Maryland and other states. He is dedicated to fighting for justice, and welcomes the opportunity to help you.
About the Nurse Consultant
La kesha Dillard, started her nursing career in 1994 as a Home Health Aide (HHA). She enjoyed working with people so much that she earned her certification as a Certified Nursing Assistant (CNA). She attended Trocaire College and completed both (the LPN and RN) programs where she earned her LPN/RN AAS degree. She was motivated to further her education and in 2016 she received her baccalaureate degree in nursing from Daemen College Amherst, NY. In 2019 she successfully completed Chamberlain College of Nursing, Nurse Executive and Leadership program, and earned a Masters of Science in Nursing (MSN) degree.
Mrs. Dillard wanted to learn more about the business side of nursing, so she attended Devry University and received her Master of Business Administration (MBA) degree in 2023.
In 2021, she successfully completed the Vicky Millazo program where she earned her certification as a Legal Nurse consultant. She opened up her nurse consulting business in 2022 and is the proud owner, founder/CEO at Mrs. RN Consulting, LLC. La kesha has consulted and worked with many attorneys by helping them understand the medical records to get justice for their clients. She has worked at several Long-Term Care facilities (LTC), medical surge units and has several years of experience with patient care and consulting.
She is a strong advocate for patients and believes in Person-Centered Care (PCC) at all times. La kesha is also a tough upholder for staff rights, and she continues to motivate nurse entrepreneurs to further their education in nursing.
Medical Malpractice & Nursing Home Lawyer Near You in Baltimore, Maryland & Beyond
I can help you anywhere in Maryland, including Allegany County, Anne Arundel County, Baltimore City, Baltimore County, Carroll County, Calvert County, Caroline County, Cecil County, Charles County, Dorchester County, Frederick County, Garrett County, Harford County, Howard County, Kent County, Montgomery County, Prince George’s County, Queen Anne’s County, Somerset County, St. Mary’s County, Talbot County, Washington County, Wicomico County, and Worcester County.
I have helped clients in over a dozen jurisdictions, including California, Delaware, District of Columbia, Georgia, Illinois, Iowa, Massachusetts, Maryland, Mississippi, New Jersey, New Mexico, New York, North Carolina, Pennsylvania, South Carolina, Washington, and Virginia.
I help injured victims nationwide in all 50 states on a case-by-case basis via Pro Hac Vice.