Article Updated: November 14, 2023
Nursing Home Bed Sores
Nursing homes are terrible at preventing bed sores, because their #1 priority is making money, and that means cutting corners. When corners are cut, nursing home residents:
◊ Do not get turned and repositioned enough
◊ Do not get adequate nutrition
◊ Do not get monitored and evaluated comprehensively for updated care planning
And when those things do not happen, innocent people die.
I have investigated over 50 cases where nursing home bed sores killed the resident, so I know this issue inside out.
Below, I walk you through the issue to answer the most common questions concerning nursing home bed sores.
If you have questions after reading the article or need legal help, reach out to me day or time, I am here for you.
Clickable Table of Contents
Nursing Home Bed Sores Legal Issues
1 – Nursing Home Bed Sore Claims
2 – Can You Sue a Nursing Home for Bed Sores
3 – Nursing Home Bed Sores Lawsuit
4 – Is Bedsores Neglect
Nursing Home Bed Sores Medical Issues
5 – Bed Sores in Nursing Home Patients
6 – What Causes Bed Sores in Nursing Homes
7 – Preventing Bed Sores in Nursing Homes
8 – Surgery for Pressure Ulcers in Nursing Home
9 – Surgery for Pressure Ulcer Q&As
Resources
10 – Nursing Home Bed Sores Legal Help
11 – Supporting Literature, Citations & Research
12 – About the Author
13 – Legal Help in Maryland & Nationally
Nursing Home Bed Sore Claims
Nursing home bedsore claims result from negligence in a majority of cases. It is the lack of proper care and staffing that leads to residents being left unmoved which causes the bedsores to develop.
You can sue a nursing home for a bedsore but it does require you to show that the nursing home is liable and that they acted in a way that was ineffective and led directly to the bedsore injuries.
The lawsuit can come directly from the patient themselves or their surviving family members if the patient passes away.
What Happens When You Develop A Bedsore?
Nursing home bed sores develop when a person has segments of their body that for too long are left unmoved.
When this happens, there is friction on the skin and over time this skin breaks down and become open ulcers. These open wounds then become infected which can lead to blood poisoning and even death.
In many cases, a bedsore can lead to the need for surgery and intensive long-term care.
Bedsores tend to develop on areas like the lower back, heels of the foot, buttocks and shoulder blades. The reason these body parts are affected is because a person laying down for long periods of time will have pressure placed on these parts for long periods of time.
Once the bedsore starts to develop, it will go through stages. There are 4 stages of a bedsore and when your body starts on stage 1 there is considerable time before the bedsore develops into the more serious later stages.
If, however, there is a total failure to turn and reposition a resident, I have seen instances where a bed sore reaches stage 4 in a matter of weeks.
In the initial stage, you will develop skin that starts to turn red but will not break. It will be the later stages where the skin starts to erode away.
Going from a stage 1 bedsore to a stage IV bedsore can take anywhere from a few weeks, to months, to over a year.
What this means is that considerable neglect goes into treatment that allows a stage 1 bedsore to get so bad to become a stage III or IV bedsore. It is not a singular incident of negligence, but a systemic, pattern of negligence which causes bed sores in a nursing home setting.
Physical Effects Of A Bedsore
The physical effects of a nursing home bed sore can be highly painful and even lead to death. A bedsore not only causes discomfort from the initial sore but also because of the potential for it to get infected which leads to a chain effect of medical problems.
A person with a bedsore will also have a constant foul odor as the skin in the affected areas is literally rotting away leaving them with decayed flesh on their body.
The physical effects, their pain and the length of time that it takes to treat a bedsore are all part of the reason that you can sue in a bedsore case in a nursing home.
Neglect is the major allegation because it is known that considerable time is needed for bedsores to develop and in order for one to get to stages III-IV means lack of care, lack of attention and often lack of nutrition and hydration.
The medical reality in a bedsore case is that it is not an unforeseen event and in fact specific care standards are in place to ensure that they do not occur.
If a bedsore has reached a higher stage of severity, this on its own suggests high levels of neglect and poor standards of care.
Can You Sue a Nursing Home for Bed Sores
Stage I-II Bedsores
Stages matter in deciding whether or not your case should go to court. The IV stages of bedsores each have distinct characteristics and it is these characteristics that will make going to court either worthwhile or not.
One of the reasons that a stage I-II bedsore is not worth the long-term court battle is that it will take longer to be in court and cost more to deal with the lawsuit than can likely be recovered.
A stage III-IV on the other hand is more likely to have a higher payout in your medical malpractice lawsuit. It is precisely because of the length of care and the cost of care, which are both high, that it makes sense to go for a lawsuit.
The stages of the bedsore and the viability of going to court for each are:
◊ Stage I: slight reddening and potential change of texture in the skin as well as slight skin irritation. This is not usually a good case for a lawsuit.
◊ Stage II: Skin will start to have more discoloration and potentially start to have pus and partially ruptured skin. While this is more painful, it can be treated well at this stage and is still not the most viable lawsuit case.
◊ Stage III: Skin will start to be damaged and look cratered like it is collapsing. In this stage there will often be strong odor, draining from the wound and the area will feel hot. At this stage, the risk for infection will be higher. Once a bedsore has reached stage III, it is a higher contender for a lawsuit.
◊ Stage IV: Skin will be red and potentially black from the areas of skin that are dying off. You can expect a considerable amount of pus and draining as well as strong odour from the wound. A person at this stage will have a high chance of fever and infection and the condition can be life-threatening. A stage IV bedsore is always an ideal case to take to court, and at the least is deserving of a medical merit review unless there are obvious indicators that the wound was not preventable.
Stage III-IV Bedsores
Stages III-IV of a bedsore are very serious and often cause the patient to die if he or she is over the age of 75. When a person has reached this level of a bedsore, they have clearly worked their way from stage I to stage II and then to stage III or IV, over the course of weeks or months of neglectful care.
This takes time, and having reached stage III and IV means that a person was neglected and their care was inadequate and, indeed, reckless.
Standards of care in nursing homes specifically ask that patients who are bound to a bed are moved every 2 hours. For a person to get to the point of stage III-IV means that they were not only not moved in an adequate manner to be up to medical standards, but that their condition was ignored as it progressed.
This level of neglect is about more than just the failure to move the patient. There is also a correlation between dehydration and malnutrition in bedsore cases, which means that a person who has reached this level of a bedsore has been neglected in more than one way.
Deciding To Sue For A Bedsore
A few variables should be considered when thinking about whether or not you should sue in a bedsore case. One major one which has been explained, is which level of bedsore a patient has gotten to. While a stage I-II is not always the best case for a lawsuit, a stage III-IV is a good case for a lawsuit.
Another variable should be if you needed surgery for a pressure ulcer. In cases where surgery was needed, there is more invasive treatment needed which can both be costly and also painful.
Still another variable to consider is whether or not the nursing home has any evidence that they had attempted to create a care plan at all when the patient was at a stage I-II in their bedsore. Lack of any medical care at stage I-II shows complete lack of care, and that adds value to the potential recovery.
Many patients die because of their bedsores and any case which has led to death and a bedsore was involved, is a reason to elevate a bedsore case to a full litigation investigation.
Nursing Home Bed Sores Lawsuit
A medical malpractice case against a nursing home for a bedsore has its own unique stages to go through before it comes to a conclusion. While it shares some similarities with other medical malpractice cases, a bedsore case is a unique situation which does require specific care.
In a nursing home pressure ulcer case, you will face a nursing home which more often than not, will claim that they did everything they could to ensure high standards of care. They will also work hard to prove that the patient’s bedsore case was unavoidable.
It is likely that, statistically speaking, the nursing home will not be correct. Nonetheless, you will have to prove that they were negligent and this is not easy, and it is costly financially.
Stages of the Bedsore Lawsuit
What can you expect in a nursing home bedsore case? While each case will be different, a few events will take place in nearly all cases:
◊ Initial consultation with an attorney
◊ An investigation and collection of evidence including medical records and photos as well as statements from the nursing home staff and medical providers
◊ A tribunal or hearing on the case in its initial stages (often optional or waivable)
◊ Discovery so that all relevant information from the nursing home, its staff and doctors can be obtained regarding the pressure ulcer
◊ Deposition to formally collect and record evidence. This is where the evidence of expert witnesses that we collect will be used.
◊ Settlement or trial: This will be the final stage in which either the nursing home settles with you for your case, or there is a final push to go to court for a trial in the case.
The length of time it takes to get from the initial consultation to the final trial will depend on your case and while there are variations in time, generally this can take anywhere from 2 1/2 years to 3 1/2 years.
Pressure Ulcer Lawsuits & Surgery
Aggravating variables will make the need for a nursing home bed sore lawsuit higher and also make potential payouts higher as well.
If you needed surgery for example, there will be a higher likelihood that you will have longer recovery and treatment time needed.
It is inevitable that you will also have more pain and discomfort as the treatments for a pressure ulcer are uncomfortable and lengthy.
Surgery in a pressure ulcer case also means that there has been more damage, the skin has been allowed to rupture and there has been a clear progression past the stage I and stage II bedsore cases and you have entered into a stage III or stage IV bedsore case.
If multiple bed sore surgeries were needed, then your medical expenses will be greater and that will increase your potential recovery.
Is A Bedsore Neglect?
Yes. In short, a bedsore is a sign in almost all cases that there has been some level of neglect which has allowed the condition to come about.
When a bedsore is present, this means that a person has not received the needed repositioning and movement that is expected for an individual who has limited mobility.
The only reason that a pressure sore can potentially not be a sign of neglect is if a person is in stage I of the bedsore and there are a variety of medical conditions affecting them and the nursing home can show clear evidence of a treatment plan to address the problem.
This however is not a common occurrence, and in most cases of bedsores, a person has been neglected and this is why the wound developed.
Standard of Care & Nursing Home Bedsores
The main reason that a pressure sore is neglect is that many medical providers and researchers in the field of medicine have made it clear that simple yet effective tools are available to prevent a bedsore.
The most obvious one is that patients need to be moved periodically.
This means that any patient in a nursing home who is not mobile, needs to be checked on and moved/ repositioned, by a member of the nursing home staff. This repositioning ensures that no one part of the body is constantly having pressure placed on it. By doing this, there is the prevention of bedsores from forming on the patient.
Other treatments are also available, such as monitoring and ensuring proper hydration and nutrition for the patient and also ensuring that there is proper medical care monitoring of the patient as well.
Adequate and appropriate food and water intake also help ensure your tissue remains hydrated and healthy, which prevents skin breakdown. Proper standard of care requires that residents be care planned to receive the right type and amount of nutrients and liquids, and if this was not done that is medical negligence.
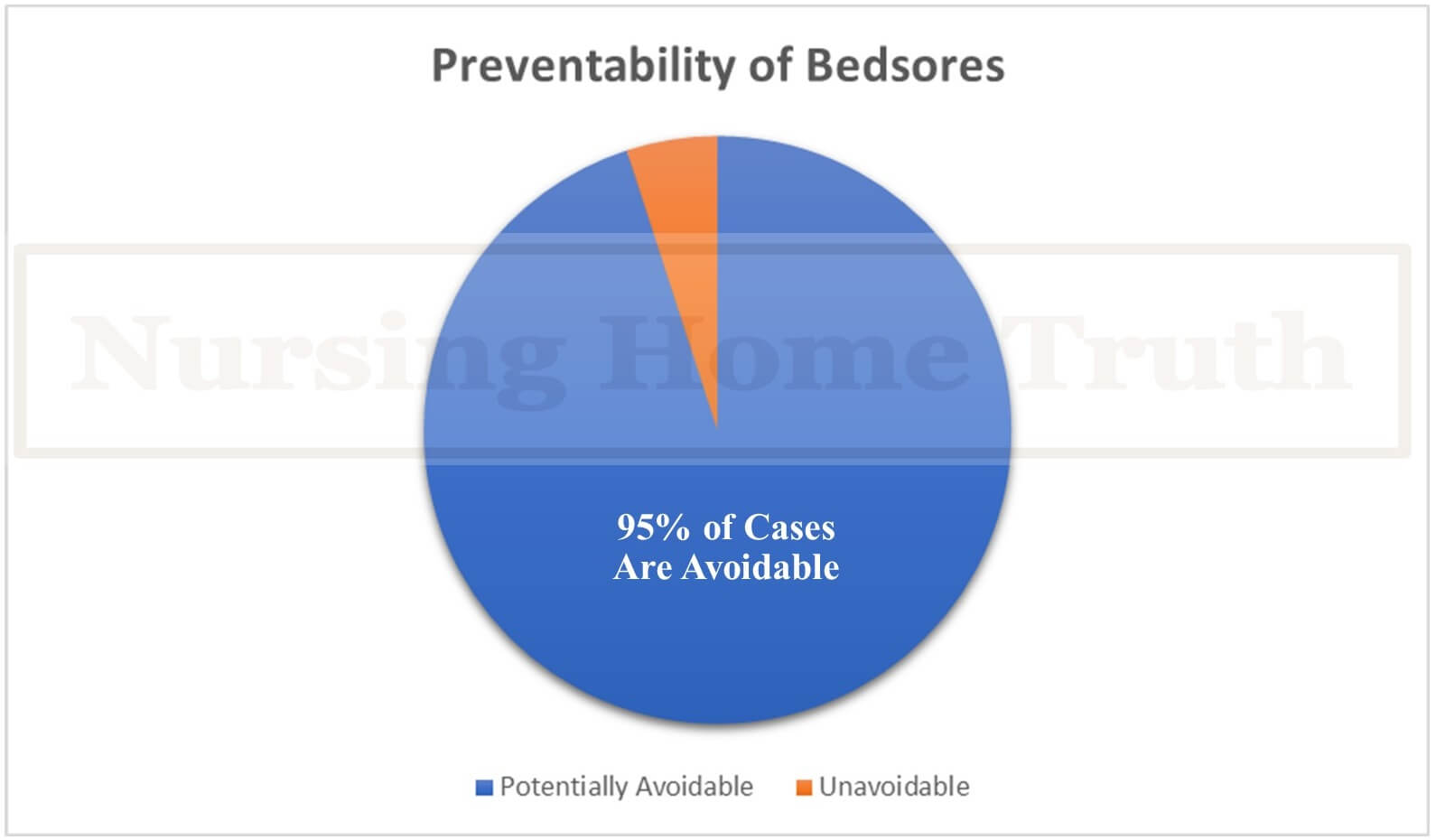
Pressure Ulcers Are Preventable
Yes, pressure ulcers are preventable and the manner in which they can be prevented is in simple acts like the repositioning of the patient. Standard of care will make a large difference in whether or not a patient will get a pressure ulcer while in a nursing home.
Research has looked directly into this and found in a study of over 364 clinical of nursing home patients with bedsores that 95% of the cases were in fact preventable. These studies have made it clear that in a majority of bedsore cases that are being seen are a result of poor treatment quality and are therefore preventable:
“Estimates show that 95% of bed sores are potentially avoidable; therefore, their appearance has a direct relationship to the quality of treatment provided.”
The preventability of pressure sores is a major reason that any pressure ulcer case that gets past a stage III should seek a litigation investigation.
Simply put, bedsores in nursing home patients generally means that neglect was present.
Bed Sores in Nursing Home Patients
Bed sores in nursing home patients are common. A major reason for this is that millions of individuals are in nursing homes and many nursing homes are crowded and understaffed.
This leads to there being higher rates of stage III and stage IV bedsore cases and more cases that need surgery for pressure ulcers as well.
Nursing Influence on Pressure Ulcers
A major influence on nursing home prevalence of pressure ulcers is in the staff that work in nursing homes. Not all nursing homes pay attention to the hiring of individuals who are experienced and understand pressure ulcers and standard of care in elderly patients.
When this happens, the attitudes and the lack of knowledge of the nurses and nursing home care staff, will have a direct impact on the prevalence and severity of the pressure ulcer cases that are going to be seen.
Crowded Nursing Homes Equal More Pressures Ulcers
When there are too many people in the nursing home and not enough nurses, there is a higher chance that there will be cases of pressure ulcers. Patients need to be turned every 2 hours and without adequate staff, there will be many lapses in treatment and this basic standard of medical care.
Fewer nurses means less time to be meticulous in ensuring that you are taking time to monitor and move each patient in the manner that is best for them and their overall physical health related to pressure ulcers.
This is made even worse in cases where a patient is in a long-term care facility as there may not be oversight and accountability in the need for repositioning on a consistent basis, which can result in a person reaching stage III or IV of a pressure ulcer.
Without this level of care and attention, a stage I or II pressure ulcer case will escalate and can turn into infection and death or mean that a person will need surgery for their pressure ulcers.
What Causes Bed Sores in Nursing Homes
Bedsores are caused by friction, malnutrition and dehydration, but more than anything else, they are caused by neglect.
A bedsore is neglect because it is preventable and the sheer fact that a person has one, in most cases, especially a bedsore above a stage II, means that there was a pattern of neglect present.
There are a few major categories of causes for bedsores we will discuss below.
Pressure & Fiction Cause Bedsores in Nursing Homes
The main physical reason that a bedsore forms is friction and pressure. When a person is laid in one position without movement for a long period of time, they will have friction, rubbing and pressure go on one part of their body. This pressure causes the skin to degrade over time and become an open wound.
This open wound is a pressure sore and when not treated immediately, the decay of the skin spreads and becomes infected which causes pus and draining.
Dehydration & Malnutrition
One manner of preventing bed sores in nursing homes is to ensure that patients are always hydrated and are being given all of their needed nutrition.
Without proper hydration and nutrition, an individual is both more susceptible to bed sores, but also less likely to be able to recover from a bedsore in its early stages.
Neglect & Crowded Nursing Homes
Most nursing home bed sores lawsuits arise because neglect is at the heart of the bedsore forming in the first place.
Not only is the neglect present in the original bedsore forming, but also in the monitoring of the bedsore to ensure that it does not get worse than a stage I or at the most a stage II.
Neglect happens for a few reasons, some of the more frequently occurring reasons are:
◊ Nursing home is crowded and staff are not able to adequately attend to the patients
◊ Nurses are not properly trained and do not know how to treat bedsore cases
◊ Patients/ residents in a nursing home are not repositioned every 2 hours
Preventing Bed Sores in Nursing Homes
Bedsores can be prevented. A few common practices can be used to ensure that bedsores are avoided or caught early on and treated in an efficient manner.
Prevention of a bedsore means that the nursing home is able to understand the needs of the patients and also make sure that they are enforcing proper care at all times to all residents.
Ensure Proper Bed Sore Care
Nursing home bed sores lawsuits can be avoided with proper care.
While this is a simple and obvious piece of advice, nursing homes fail in this as they are not always looking only at patient care, but also bottom lines which keep nursing homes understaffed or with lower quality staff.
The steps that can be taken to prevent bed sores in nursing homes are:
◊ Adequate staff are present to take care of all patients
◊ Proper nutrition and hydration are provided
◊ Ensuring proper movement which means repositioning every 2 hours to prevent bedsores
These steps can help to cut down on nearly 95% of nursing home pressure ulcer cases.
Surgery for Pressure Ulcers in Nursing Home
Some cases of pressure ulcers will get bad enough that the only way to treat them effectively will be to use surgery.
When surgery is needed, a nursing home bed sore lawsuit will take into account the treatment that was used on the patient and surgery is considered a costly and painful treatment option.
There are a limited number of options available when a person has a bedsore bad enough to require surgery. The most common ones are wound debridement, wound vac and flap surgery.
For a sizeable number of my clients, they are in such a vulnerable physical state that surgery is not an option. For these victims, the bed sore created an untreatable death sentence.
Wound Debridement
Debridement is a medical process where dead and damaged tissue and skin are removed so that the healthy surrounding tissue can recover better and not be negatively affected by the dying tissue.
Debridement can be done through a variety of methods. Different debridement methods are:
◊ Surgical Debridement
◊ Mechanical Debridement
◊ Chemical Debridement
Wound Vac
Wound vac can be used on its own, or used with debridement to help clean the affected pressure ulcer area while also at the same time draining the fluids that are present in the wound. This surgical procedure is usually reserved for more serious bedsores that are in stage III or stage IV.
The use of these wound vacs can help more serious cases with recovery as there is the removal of fluid and infection which can accumulate in the sores and make recovery harder, and also lead to the foul odor that is often found with bedsores.
Flap Surgery
Bed sores in nursing home patients can often lead to entire areas of skin becoming necrotic, which means that the skin is dying like it would on a person who has passed away. In cases this severe, dramatic options must be taken with surgery.
One such option is the flap surgery in which a pad of your own muscle or skin is cut and used to cover the affected areas that have a pressure ulcer.
If the victim underwent flap surgery, then there is a good likelihood that the claim is sufficiently viable to merit an investigation. When I say “sufficiently viable,” I’m referring to the fact that investigating these claims take thousands, and often tens-of-thousands, of dollars, so a substantial injury is necessary to compel a lawyer to spend that money on the investigation.
Nursing Home Bed Sores Q&As
Can you sue a nursing home for bed sores?
Yes, you can sue a nursing home for a bed sore. The main reason that you can sue, particularly if the bedsore is at a stage III or IV, is that the bedsore being present shows that there was some level of neglect on the part of the nursing home.
How effective are nursing home bed sores lawsuits?
Nursing home bedsore lawsuits can be effective when they are taken care of by an attorney who is experienced in cases involving nursing homes and bedsore cases. When a bedsore case is also at a stage III or higher, and there is no plan of care that was addressing the case, proving neglect can be easier as long as the proper paperwork is collected for the court case in a timely manner.
Is a bedsore considered neglect?
Yes, a bedsore can be considered neglect. Nursing homes have specific rules, laws and guidelines that determine the standards of care that they have to provide patients. Amongst these are specific rules on prevention of bedsores which includes making sure to move a patient every 2 hours so that they are not placing pressure on one part of their body alone for an extended period of time.
How common are bed sores in nursing home patients?
Bed sores are very common in nursing homes because many nursing homes are understaffed and do not follow the standards of care for repositioning residents/ patients every 2 hours which leads to the development of pressure ulcers.
What causes bed sores in nursing home patients?
The most frequent cause of pressure sores in nursing home patients is the lack of repositioning which leaves them to suffer with one part of their body constantly under pressure. This pressure causes the skin to erode and eventually leads to infections. Other causes can make this worse as well, such as lack of proper hydration and nutrition in the individual.
If I need surgery for a pressure ulcer does it affect my settlement?
Yes, the need for surgery for a pressure ulcer can affect your settlement because it shows that your pressure ulcer was at a higher stage, likely a stage III or IV, and that you needed more intensive treatment to alleviate your condition.
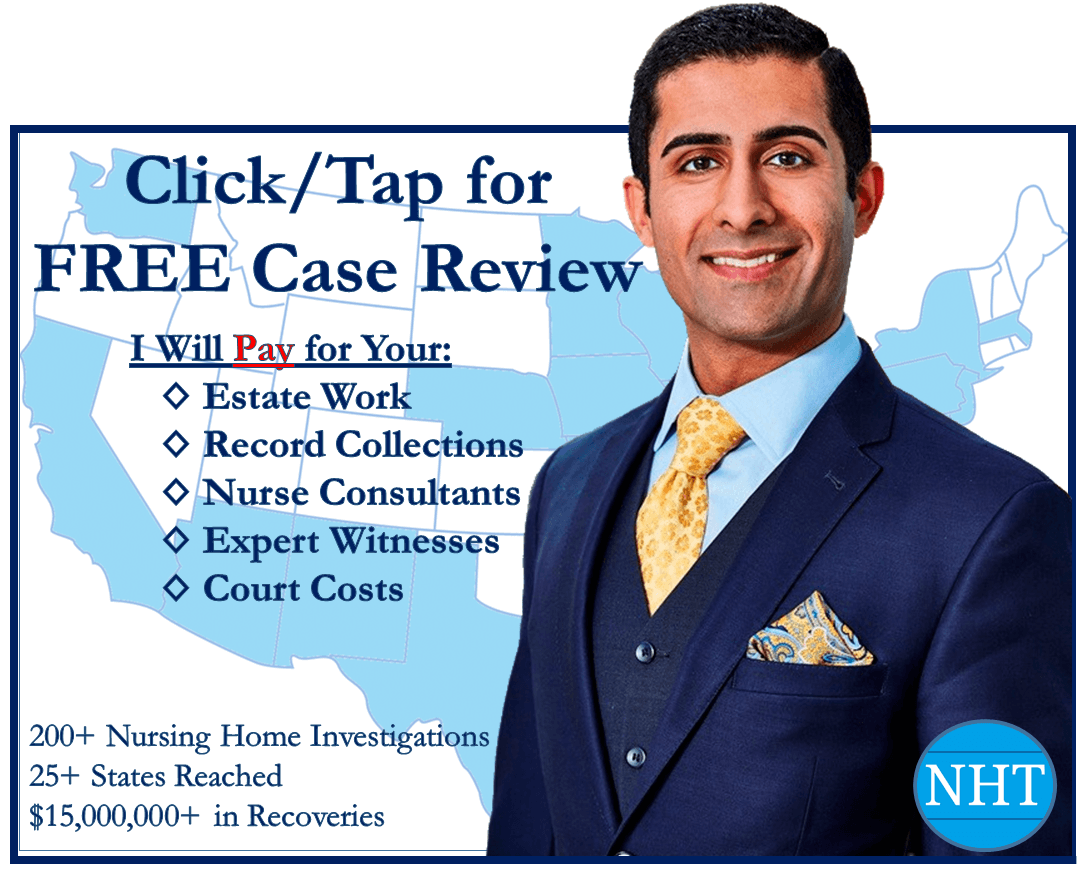
Nursing Home Bed Sores Legal Help
Nursing home bed sores are hands down the most common and deadly injury that nursing home patients suffer. A substantial majority of my nursing home clients are suffering from, or died as a result of, bed sores acquired in a nursing home.
Based on the hundreds of nursing home bed sore cases I have reviewed, I would estimate that well over 95% of the bed sores were preventable, and well over 95% of the time the nursing home’s negligence caused the bed sores.
Do not trust the nursing home’s excuses. Once they injure you, their only concern is covering up their medical crimes. Get an advocate who knows how to hold nursing homes accountable to fight for you. When you hold the nursing home accountable, you can help prevent this from happening to other vulnerable nursing home residents.
When you are ready to take the first steps towards getting justice, I am here for you. If you just want to ask questions, I am here for that, too.
Warmly,
Reza Davani, Esq.
State Bar No.: #1212110211
Federal Bar No.: #30168
Cellphone: (301) 922-4598
Email: reza@nursinghometruth.com
Pressure Ulcer Legal Library
Click/Tap Icons to Access Articles

Supporting Literature, Citations & Resources:
Assefa, T., Mamo, F., & Shiferaw, D. (2017). Prevalence of bed sore and its associated factors among patients admitted at Jimma University Medical Center, Jimma Zone, Southwestern Ethiopia, 2017 cross-sectional study. Orthopedics and Rheumatology Open Access Journals, 8(4), 74-81.
Park-Lee, E., & Caffrey, C. (2009). Pressure ulcers among nursing home residents; United States, 2004.
Demarré, L., Vanderwee, K., Defloor, T., Verhaeghe, S., Schoonhoven, L., & Beeckman, D. (2012). Pressure ulcers: knowledge and attitude of nurses and nursing assistants in Belgian nursing homes. Journal of clinical nursing, 21(9‐10), 1425-1434.
Flynn, L., Liang, Y., Dickson, G. L., & Aiken, L. H. (2010). Effects of nursing practice environments on quality outcomes in nursing homes. Journal of the American Geriatrics Society, 58(12), 2401-2406.
BoykoTatiana, V., LongakerMichael, T., & YangGeorge, P. (2018). Review of the current management of pressure ulcers. Advances in wound care.
White-Chu, E. F., Flock, P., Struck, B., & Aronson, L. (2011). Pressure ulcers in long-term care. Clinics in geriatric medicine, 27(2), 241-258.
Levine, S. M., Sinno, S., Levine, J. P., & Saadeh, P. B. (2013). Current thoughts for the prevention and treatment of pressure ulcers: using the evidence to determine fact or fiction. Annals of surgery, 257(4), 603-608.
Leyva-Moral, J. M., & Caixal-Mata, C. (2009). Prevalence of bed sores in geriatrics nursing home residences. Revista de enfermeria (Barcelona, Spain), 32(1), 52-56.
About the Author
This nursing home and medical malpractice article was written by Baltimore, Maryland nursing home attorney Reza Davani, Esquire. Mr. Davani received his Juris Doctor degree from a Tier 1 law school, the University of Maryland Francs King Carey School of Law. He received his first license to practice law from the State of Maryland’s Court of Appeals (MD State License No. 1212110211), and just four months later received a federal law license from the United States District Court for the District of Maryland (Federal License No. 30168).
Mr. Davani has been practicing law for over 10 years. He began practicing law by helping clients as a sanctioned student lawyer before receiving his law license, and second chaired his first jury trial in federal court before even graduating law school. He is a registered member of the Maryland Association for Justice (MAJ), the American Bar Association (ABA), the American Association for Justice (AAJ), and was formerly on the MAJ’s Legislative Leader’s Circle.
Mr. Davani has taken over 20 cases to trial in state and federal court, and favorably settled well over 100 cases for injured victims. He has personally helped his clients recover over $15,000,000 in personal injury, medical malpractice, and nursing home abuse settlements and verdicts in Maryland and other states. He is dedicated to fighting for justice, and welcomes the opportunity to help you.
About the Nurse Consultant
La kesha Dillard, started her nursing career in 1994 as a Home Health Aide (HHA). She enjoyed working with people so much that she earned her certification as a Certified Nursing Assistant (CNA). She attended Trocaire College and completed both (the LPN and RN) programs where she earned her LPN/RN AAS degree. She was motivated to further her education and in 2016 she received her baccalaureate degree in nursing from Daemen College Amherst, NY. In 2019 she successfully completed Chamberlain College of Nursing, Nurse Executive and Leadership program, and earned a Masters of Science in Nursing (MSN) degree.
Mrs. Dillard wanted to learn more about the business side of nursing, so she attended Devry University and received her Master of Business Administration (MBA) degree in 2023.
In 2021, she successfully completed the Vicky Millazo program where she earned her certification as a Legal Nurse consultant. She opened up her nurse consulting business in 2022 and is the proud owner, founder/CEO at Mrs. RN Consulting, LLC. La kesha has consulted and worked with many attorneys by helping them understand the medical records to get justice for their clients. She has worked at several Long-Term Care facilities (LTC), medical surge units and has several years of experience with patient care and consulting.
She is a strong advocate for patients and believes in Person-Centered Care (PCC) at all times. La kesha is also a tough upholder for staff rights, and she continues to motivate nurse entrepreneurs to further their education in nursing.
Nursing Home Bed Sores Lawyer Near You in Baltimore, Maryland & Beyond
I can help you anywhere in Maryland, including Allegany County, Anne Arundel County, Baltimore City, Baltimore County, Carroll County, Calvert County, Caroline County, Cecil County, Charles County, Dorchester County, Frederick County, Garrett County, Harford County, Howard County, Kent County, Montgomery County, Prince George’s County, Queen Anne’s County, Somerset County, St. Mary’s County, Talbot County, Washington County, Wicomico County, and Worcester County.
I have helped clients in over a dozen jurisdictions, including California, Delaware, District of Columbia, Georgia, Illinois, Iowa, Massachusetts, Maryland, Mississippi, New Jersey, New Mexico, New York, North Carolina, Pennsylvania, South Carolina, Washington, and Virginia.
I help injured victims nationwide in all 50 states on a case-by-case basis via Pro Hac Vice.