Article Updated: April 3, 2022
UTI Death in Nursing Home
Having handled well over 500 nursing home litigation investigations and claim reviews, I have a good sample size based upon which I can make this observation:
Right behind bed sores, UTI death claims are probably the #2 most common category of injuries and claims that victims call me about.
I suspect it’s because nurses, who are short-staffed because of greedy nursing homes, deal with the most obvious fire they can see, and UTI death symptoms are often more discreet than, say for example, a resident that is choking on her dinner or a stage IV bedsore that is oozing blood.
Nonetheless, these UTI death incidents are happening at a high frequency, and must be investigated. As I write these very words, I am in heated litigation with two separate nursing homes over UTI death cases.
Below, you will learn more about UTI death claims and UTI injuries in the nursing home setting. If you have questions after reviewing my writeup, you are invited to call me for a free consultation.
Clickable Table of Contents
UTI Death & Causes in Nursing Homes
1 – Causes of UTIs In Nursing Homes
2 – How To Prevent UTI In Nursing Home
3 – Nursing Home Negligence UTI
4 – UTI Deaths Frequency?
5 – Q&A On Causes Of UTIs In Nursing Homes
Resources
6 – Get Help With Your Nursing Home Negligence UTI Case
7 – Supporting Literature, Citations & Research
8 – About the Author
13 – Legal Help in Maryland & Nationally
Causes of UTIs In Nursing Homes
Many of the major causes of UTI in nursing homes are preventable meaning millions suffer every year from a painful condition when they do not have to.
At all age groups people are susceptible to a UTI and it generally involves bacteria like Escherichia coli and Enterococci and Staphylococci as the main culprits for the infections.
Bacteria are not the only organism that can cause a UTI, but they are the most common cause for most UTIs, particularly in nursing homes.
UTI Death Caused by Hygiene Shortcomings
One major of the major causes of UTI deaths and injuries in nursing homes is poor hygiene.
When an individual is exposed to infections like Escherichia coli (E. coli), Chlamydia, and mycoplasma bacteria that enters into their urinary tract, they will develop an infection that often times ends up becoming a long-term problem for them.
But why does this happen so frequently?
In long-term care homes many residents need to wear diapers or have catheters, and when these are not cleaned or changed in a timely and hygienic manner, it leads to the spread of infections.
Additionally, in care homes there are often many individuals with varying infections and poor hand washing and basic hygiene practices lead infections to get out of hand.
As there are also many residents who are immobile, being left in unhygienic conditions where they are not moved frequently enough, taken to the battle frequently enough or showered as well as they should be, the spread of infections like UTIs becomes more common.
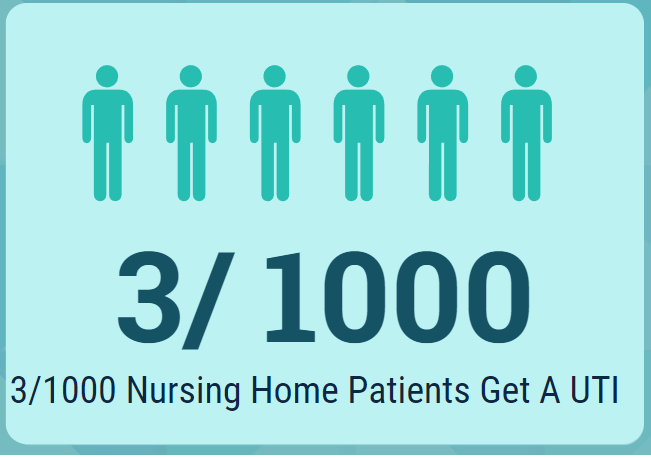
The problem is so frequent that in an average nursing home in the U.S. it is expected that at least 3 out of every 1000 residents will contract a serious UTI infection at any given point and time.
UTI Death Caused by Poor Catheter Management
For many in nursing homes, catheters are a necessity. Catheters can cause many problems ranging from benign ones, to ones so serious that you can suffer a UTI related death.
According to the National Healthcare Safety Network UTIs are common and over 70% of them are linked to a urinary catheter.
A urinary catheter is placed inside the urethra and connects to the bladder to help drain urine for those whose bodies cannot do this on their own.
These types of UTIs are common in both inpatient and outpatient settings.
These catheters cause a UTI because of lack of cleanliness or improper use.
In nursing home residents this is a serious situation as these catheter related UTIs are a common cause of sepsis, hospital admission, and antimicrobial use that leads to patients being given too many medications that can lead to drug-resistance.
Catheter problems increase the chances of UTI and reports have found for serious infections, such as S. aureus bacteremia, led to UTI deaths for almost 36% of those who suffered a UTI infection of this sort.
In addition to being common and dangerous, a UTI that comes from a catheter is also more likely to be difficult to treat.
When this happens infections can spread from the urinary tract system into other areas of the body like the kidneys.
UTI Death & Injury from Over-Medication
A frequent problem in nursing homes is that infections are not caught fast enough and this leads to infections that last longer than they should before being treated.
Despite studies showing that for 30 years one of the most consistently common infections among NH residents are UTIs there is still not enough knowledge amongst nursing staff to catch UTIs in a timely manner.
When an infection is finally caught, there is a large reliance on overmedicating the patient and this causes more UTIs and antibiotic-related harms. This harm is not only in the individual who has the UTI, but also others residing within the same nursing home.
The reason for this is that this overmedication tendency leads to the development of stronger, more virulent and difficult to treat strains of UTI.
Failing to identify infections is itself linked to poor nursing practices and can be seen as a form of nursing home negligence regarding UTIs.
How To Prevent UTI In Nursing Home
Knowing how to prevent UTIs in a nursing home is an imperative part of best practices that nurses are responsible for.
It is not always an easy task to stop a UTI, but despite the difficulty, many methods are available to help nurses and nursing home staff take action to mitigate the spread of infections.
Prevent UTI by Recognizing Symptoms Quickly
One way that nurses can help prevent UTIs is to actually identify them as soon as possible in a patient that does have a UTI.
The key is stopping the spread of the UTI to more residents.
Those who live in nursing homes are in constant contact with each other and when an undiagnosed case of UTI is allowed to fester, it can only mean a stronger infection and one that can cause a problem for others in the nursing home as well.
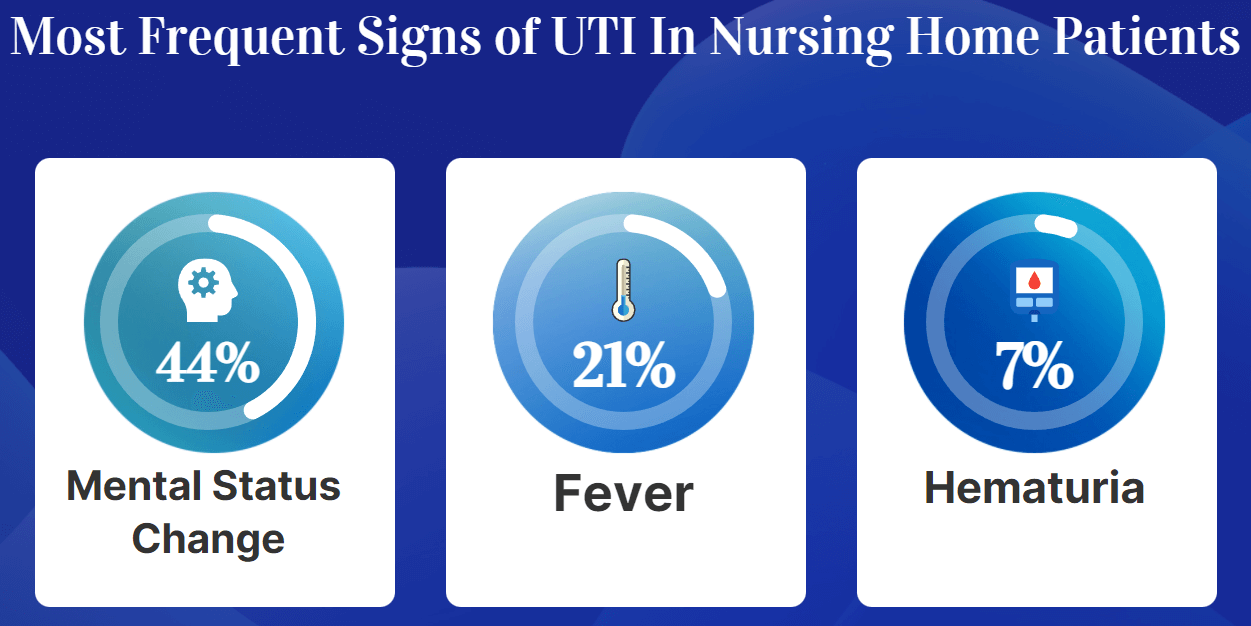
Nurses have many ways to identify whether or not a UTI may be present. They can look for symptoms such as:
◊ Mental status change (seen in 44.3% of those with UTI infections)
◊ Fever (Found in 20.6% of patients)
◊ Hematuria or blood in the urine (6.9% showed this symptom)
◊ Dysuria or painful urination (3.8% of instances of UTI amongst residents)
◊ Costovertebral Tenderness or Kidney pain (2.3%)
◊ Urinary frequency (1.5%)
◊ Chills or rigor (1.5%)
Prevent UTI by Minimizing Dehydration
Minimizing dehydration is another way you can prevent UTIs in nursing homes.
The connection between lack of adequate fluids and infections in the urinary tract are high.
Harvard Medical School has noted itself that studies show more water means less dehydration and less dehydration means fewer cases of UTIs, especially the more serious UTI called cystitis.
Being hydrated also means that when an individual does develop a UTI, they are less likely to be in need of antibiotics than those who are dehydrated.
Women in particular benefit from higher levels of hydration as it is closely related to the chances that they will develop a UTI while in a nursing home.
Prevent UTI by Providing Adequate Bathroom Access
If you have little knowledge of UTIs or if you are not sure how to prevent UTIs in nursing homes the most important piece of advice will be use of the bathroom.
Having access to the bathroom and using it frequently can mean the difference between common UTI problems, and avoiding such a painful infection.
It is a myth that if you do not use the bathroom you will develop a UTI. Holding it is not what causes the infection, a bacteria or other organism on the other hand does cause a UTI.
When you hold it, or are denied access to a restroom in a timely or regular manner, it is more likely that the bacteria that is in your bladder will sit there and multiply. This is what can cause a UTI to develop.
Being denied access to a restroom is another form of nursing home negligence that can lead to a UTI.
Prevent UTI via Proper Medication
Prescribing medication correctly can reduce UTIs in nursing home residents.
Prescriptions being given in an incorrect manner leads to antibiotic-related harms and an increase in medication resistance in trains of UTIs.
Very often, lack of knowledge of UTI cases and lack of proper communication skills in staff can influence the diagnosis of an infection and lead to delays in infection treatment as well as the wrong medications being given to residents.
One way that medications processes
Increasing rates of antibiotic resistance have also resulted in a shift all over the U.S. that has promoted proper medication usage in cases of UTIs as being a reduction in medication usage.
It is only in this reduction of medication reliance that there can be prevention of the continued development of strong strains of bacteria that are linked to higher infection rates and UTI death rates.
Nursing Home Negligence UTI
When there is a suspected UTI in a nursing home a physician rarely visits. Instead, the influence and communication of the UTI being treated comes down to the knowledge of UTIs that the nurses have and relay to the physician.
Nurses Are Main Point of Contact On UTIs
Since nurses are the main point of contact on treatment and identification of a UTI, their level of knowledge will wholly impact what happens to a nursing home resident who has this infection.
Nurses have been found to be the central decision-maker in treatments i.e. prescribing of an antibiotic or ordering another course of action.
So trusted are nurses in this regard that a large number of doctors reported that they accepted the nursing staff’s assessment of a resident and seldom visited a patient in a nursing home for a UTI.
Hiring poorly trained or incompetent nurses itself is therefore nursing home negligence on UTIs as patients are left in the hands of these nurses with little oversight by doctors on what is being done to treat a UTI.
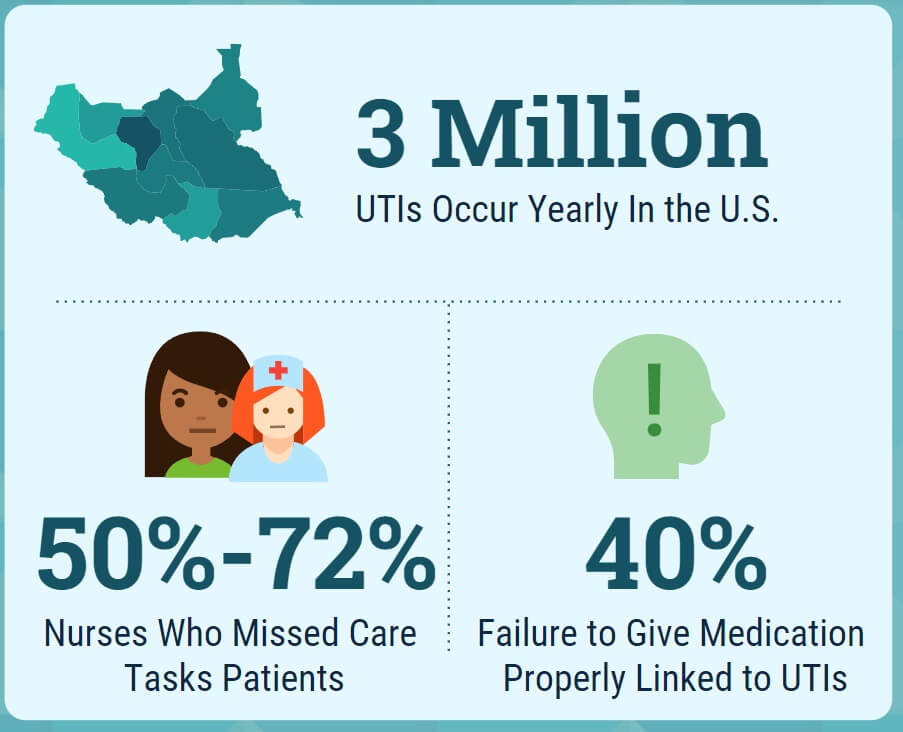
This negligence is even more evident when you see that nearly one half of nurses reported missing at least important and necessary care activity that they needed to provide their patients during their last shift.
More shocking that this is that out of the 12 categories of reported missed care activities, “seven categories of missed care were significantly correlated with UTIs”.
In fact, high rates of poor UTI control in nursing homes are related to failure to administer medications on time and failure to provide adequate patient surveillance, which explained 40% high rates of UTI in nursing home residents.
Nurses Lead UTI Prevention & Mitigation
Nurses are the main prevention gatekeepers for UTIs in nursing homes.
One thing that nurses can do is make sure that they are keeping their eyes open for UTIs because often, the symptoms and signs of a UTI that are needed to start treatment are frequently absent in NH residents, especially those with cognitive concerns like dementia.
In cases like this, nurses will need to be diligent in identifying and treating UTI infections.
Certified nursing assistants (CNA) can also help support the prevention of UTIs in many ways.
This includes:
◊ Making sure that residents have access and assistance to the bathroom every 2-4 hours
◊ Ensuring that patients are offered water and hydrated at all times
◊ Providing proper catheter care
◊ Promoting and following proper hand hygiene
Failure to provide simple mitigation methods like these can lead to the spread of serious UTI infections.
How Frequent are UTI Deaths?
UTI death comes from not just the bacteria itself that causes the UTI, but the many adjacent problems that accompany a UTI.
A UTI can be missed which can allow the infection to spread to the kidneys for example, which can cause damage to the kidneys as well as the development of stones.
Furthermore, missed or ignored UTIs can also lead to serious infections that can cause pain and also infections that are septic and can lead to death.
In many cases of UTIs, it is missed care that leads to the UTI infection which leads to intense pain and advanced infection rates which in turn lead to higher chances of serious infections that can cause UTI related death.
I searched far and wide for good data on freauency on UTI deaths, but I didn’t find anything reliable enough that I felt comfortable sharing it here.
Based on my own litigation practice, reviewing hundreds of thousands of medical records which include UTI injuries, reading autopsy reports, and analyzing death certificates, I can say this. UTIs are a contributing factor to death in at least 10% of my nursing home cases.
Read that carefully – I’m not saying “the” cause or “the only” cause. I am saying a contributing cause, so UTI death cases usually have an additional injury component that also contributed to the eventual death of the resident or patient. Again, this is in my experience.
Q&A On Causes Of UTIs In Nursing Homes
What are the causes of UTIs in nursing homes?
The causes of UTIs in nursing homes are often related to incorrectly used catheters, poor access to bathrooms, dehydration and improper medication usage.
Do nurses know how to prevent UTIs in nursing homes?
Yes, nurses do know how to prevent UTIs in nursing homes which includes making sure that residents are always hydrated and making sure that they also have access to bathroom facilities as well. Additionally, nurses can also ensure fewer UTIs by making sure that proper hygiene standards are always in practice.
Can nursing home negligence cause a UTI?
Negligent care by nurses can cause a UTI to develop and also can lead to a serious infection when a UTI is not identified quickly and treatment is delayed, or improper.
Do I need law help if I believe there are excessive UTIs in a nursing home?
If you believe that there has been a mistake made in diagnosis or treatment that led to a UTI case then you should seek out legal help. An attorney can assist you as you work towards recovering damages for the pain and suffering you or a loved one suffered due to the negligence of a nursing home and its employees.
Can antibiotic overuse be considered a form of nursing home negligence in UTI cases?
The overuse of antibiotics can lead to the development and spread of drug-resistant bacteria that can spread through a nursing home population. It is the job of nursing home staff to safely and properly administer drugs in the best interest of their patients and when they fail to do this, it can be seen as a form of negligence.
Get Help With Your Nursing Home Negligence UTI Case
Nursing homes owe you and your loved ones a duty of care that demands UTIs be identified and treated effectively and quickly.
Excessive UTIs in nursing homes may mean that the nursing home broke the safety rules and caused your family to suffer avoidable harm.
You need legal help and when you feel ready to talk, I am here to offer a free consultation so you can see what your choices are.
You can reach me via private message in the contact form on this page, via email, or by calling me, at any time.
Warmly,
Reza Davani, Esq.
State Bar No.: 1212110211
Federal Bar No.: 30168

Supporting Literature, Citations & Resources:
Arnold, S. H., Jensen, J. N., Kousgaard, M. B., Siersma, V., Bjerrum, L., & Holm, A. (2020). Reducing antibiotic prescriptions for urinary tract infection in nursing homes using a complex tailored intervention targeting nursing home staff: protocol for a cluster randomized controlled trial. JMIR Research Protocols, 9(5), e17710.
Farid, H. (2018). More water, fewer UTIs? Harvard Medical School.
Nelson, S. T., & Flynn, L. (2015). Relationship between missed care and urinary tract infections in nursing homes. Geriatric Nursing, 36(2), 126-130.
White, E. M., Aiken, L. H., & McHugh, M. D. (2019). Registered nurse burnout, job dissatisfaction, and missed care in nursing homes. Journal of the American Geriatrics Society, 67(10), 2065-2071.
Schweizer, A. K., Hughes, C. M., Macauley, D. C., & O’Neill, C. (2005). Managing urinary tract infections in nursing homes: a qualitative assessment. Pharmacy World and Science, 27(3), 159-165.
Agata, E. D., Loeb, M. B., & Mitchell, S. L. (2013). Challenges in assessing nursing home residents with advanced dementia for suspected urinary tract infections. Journal of the American Geriatrics Society, 61(1), 62-66.
Mody, L., Greene, M. T., Meddings, J., Krein, S. L., McNamara, S. E., Trautner, B. W., … & Saint, S. (2017). A national implementation project to prevent catheter-associated urinary tract infection in nursing home residents. JAMA internal medicine, 177(8), 1154-1162.
Gupta, K., Grigoryan, L., & Trautner, B. (2017). Urinary tract infection. Annals of internal medicine, 167(7), ITC49-ITC64.
Agarwal, M., Dick, A. W., Sorbero, M., Mody, L., & Stone, P. W. (2020). Changes in US nursing home infection prevention and control programs from 2014 to 2018. Journal of the American Medical Directors Association, 21(1), 97-103.
Beck-Sague, C., Villarino, E., Giuliano, D., Welbel, S., Latts, L., Manangan, L. M., … & Jarvis, W. R. (1994). Infectious diseases and death among nursing home residents: results of surveillance in 13 nursing homes. Infection Control & Hospital Epidemiology, 15(7), 494-496.
About the Author
This nursing home and medical malpractice article was written by Baltimore, Maryland nursing home attorney Reza Davani, Esquire. Mr. Davani received his Juris Doctor degree from a Tier 1 law school, the University of Maryland Francs King Carey School of Law. He received his first license to practice law from the State of Maryland’s Court of Appeals (MD State License No. 1212110211), and just four months later received a federal law license from the United States District Court for the District of Maryland (Federal License No. 30168).
Mr. Davani has been practicing law for over 10 years. He began practicing law by helping clients as a sanctioned student lawyer before receiving his law license, and second chaired his first jury trial in federal court before even graduating law school. He is a registered member of the Maryland Association for Justice (MAJ), the American Bar Association (ABA), the American Association for Justice (AAJ), and was formerly on the MAJ’s Legislative Leader’s Circle.
Mr. Davani has taken over 20 cases to trial in state and federal court, and favorably settled well over 100 cases for injured victims. He has personally helped his clients recover over $15,000,000 in personal injury, medical malpractice, and nursing home abuse settlements and verdicts in Maryland and other states. He is dedicated to fighting for justice, and welcomes the opportunity to help you.
Nursing Home Abuse Lawyer Near You in Baltimore, Maryland & Beyond
I can help you anywhere in Maryland, including Allegany County, Anne Arundel County, Baltimore City, Baltimore County, Carroll County, Calvert County, Caroline County, Cecil County, Charles County, Dorchester County, Frederick County, Garrett County, Harford County, Howard County, Kent County, Montgomery County, Prince George’s County, Queen Anne’s County, Somerset County, St. Mary’s County, Talbot County, Washington County, Wicomico County, and Worcester County.
I have helped clients in over a dozen jurisdictions, including California, Delaware, District of Columbia, Georgia, Illinois, Iowa, Massachusetts, Maryland, Mississippi, New Jersey, New Mexico, New York, North Carolina, Pennsylvania, South Carolina, Washington, and Virginia.
I help injured victims nationwide in all 50 states on a case-by-case basis via Pro Hac Vice.