Article Updated: November 14, 2023
How Often Should Nursing Homes Change Diapers
Due to continence issues, many nursing home residents wear diapers. So the questions arise:
◊ How often should nursing home residents’ diapers be changed?
◊ Do inadequate diaper changes cause bed sores?
◊ Is infrequent diaper changing negligence?
Below, you will learn how diaper changes in a nursing home setting can be evidence of neglect and violations of proper medical standards.
If you have more questions or need help after reading this article, contact me day or night.
Clickable Table of Contents
Nursing Home Diaper Change Standards
1 – Diapers Worn in Nursing Homes
2 – Frequency in Changing Diapers
3 – So, How Often Should Nursing Homes Change Diapers?
4 – Neglect In Changing Diapers In Nursing Homes
5 – Consequences When Diapers Are Not Changed
Resources
6 – Get Help If Diapers In A Nursing Home Were Not Changed
7 – Supporting Literature, Citations & Research
8 – About the Author
9 – Legal Help in Maryland & Nationally
Diapers Worn in Nursing Homes
The Need for Nursing Home Diapers
In nursing homes, many individuals will need to wear diapers because of mobility issues and concerns.
Because many who live in a nursing home are not able to get up, stand up, or move around at all, they will have a diaper put on in order to address their bathroom needs.
Not all people who wear diapers in a nursing home are bedridden. Some simply have mobility issues and cannot express or control when they need to use the bathroom. Therefore, many actively mobile people also wear diapers in nursing homes.
Those who are bedridden on the other hand, or have cognitive health deterioration that prevents them from being able to control or express any need to use the bathroom, will almost always have to wear diapers at all times.
Who Commonly Wears Diapers in Nursing Homes
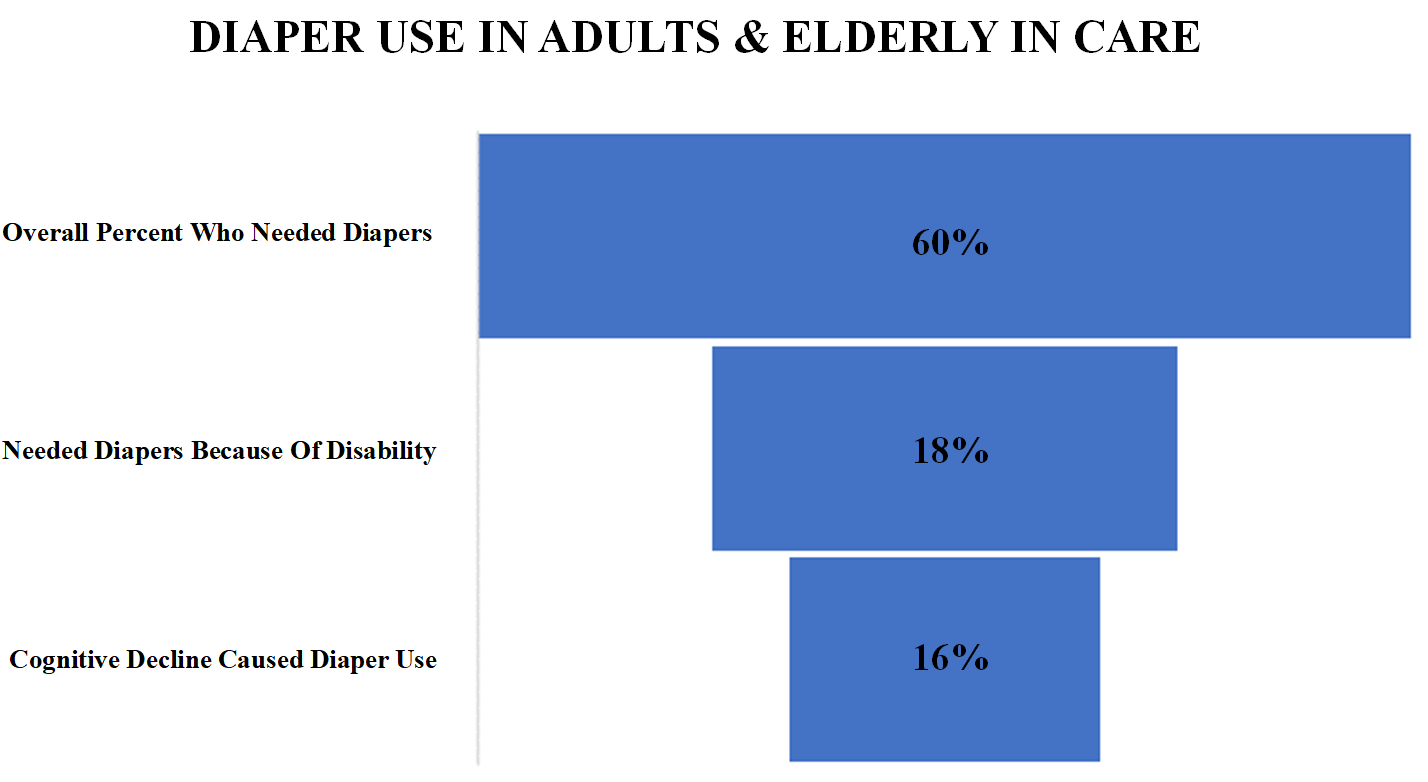
When an individual is bedridden, be it in a hospital or nursing home the need for diapers increases exponentially with many elderly in hospital care and long-term care needing diapers because of disability or cognitive decline.
Sine this is such a common occurrence, with a large majority of elderly and adults in care needing diapers at some point and time, the question then is, how often should nursing homes change diapers?
The Answer to this can vary on a number of details, but there are some overarching rules that nursing homes should generally be following in order to give their patients the best level of overall care.
Frequency in Changing Diapers
The answer to the question of how often nursing homes should change diapers is, it depends.
Incontinence and Diaper Changes in Nursing Homes
If a person has incontinence then their diaper needs to be changed far more frequently than a person who does not have any such problems. Usually, those with urinary incontinence will need to have their diaper changed at least 5-8 times in a day.
This does not mean that all incontinence is even treated the same. An individual with bowel incontinence needs to have their diaper changed immediately upon the diaper becoming soiled.
Lifestyle Impact on Diaper Changes
The biggest factor in the need for frequency in changing a diaper will be how healthy and active the lifestyle of the individual wearing diapers is.
A person who can usually get up and go to the bathroom themselves will not need to change their diaper as frequently because most of the time they will not actually use the diaper. This means that a person who has incontinence or bladder leakage can generally not need their diaper changed multiple times in a day.
This frequency changes for a person who is much older, or a person who is more severely incontinent or a person who is bedridden the majority of the day. These individuals will not be able to control their bladder long enough to get to a bathroom most of the time.
Patient’s Awareness of Bathroom Needs
Additionally, a person with this level of care needed may often not even know that they need to relieve themselves or that they have already relieved themselves.
These individuals will need to have their diapers changed far more frequently and will need to also be monitored carefully as well.
So, How Often Should Nursing Homes Change Diapers?
The answer to this question depends on which class or category of individual you are in a nursing home.
Active Individuals With Urinary Incontinence
The individuals who have bladder concerns and cannot always control or time their needs will have their diapers changed less frequently, usually once every few hours throughout the day. These are individuals who can usually voice their needs to go to the bathroom, but not all of the time.
Bedridden Individuals
A person who is bedridden needs to have their diaper changed every 2-3 hours when they have urinary incontinence. However, if an individual who is bedridden soils themselves they need to be changed as soon as possible as this can be harmful for them in the long run.
Residents With Cognitive Decline
Similar to those who are bedridden, a person with cognitive decline needs to have their diaper changed every 2-3 hours for urinary incontinence but ASAP when they have soiled themselves, otherwise major health problems can arise related to their skin.
Neglect In Changing Diapers In Nursing Homes
Inadequate Diaper Changing Equals Neglect
There is often neglect in nursing homes with regards to changing diapers in a timely manner.
Residents who cannot move or have cognitive concerns are often left with soiled or wet diapers for long periods of time which can cause health problems.
Unnecessary suffering is caused when this basic need is neglected that weighs on the emotional and physical well-being of nursing home residents.
This kind of neglect is therefore a form of abuse that many in nursing homes suffer through.
Nurse Training on Proper Diaper Changes
It is not always disregard for a resident that leads to diapers not being changed. Instead, it can often be the fault of the nursing home itself because of a lack of support and poor training that leads to unclear routines for nursing staff.
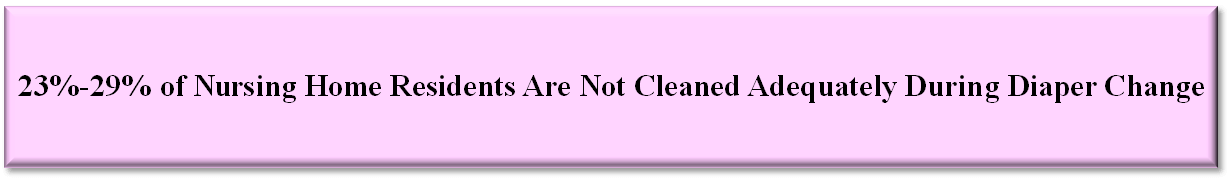
This lack of training and routine complicates the question of how often a nursing home should change diapers.
This is because even if it is done every 2-3 hours, if it is not done correctly, it is the same as not doing it at all.
When diapers are not changed properly or when they are not changed in the appropriate time intervals, there is inadequate care being given to residents. Inadequate care is very common in nursing homes and it can lead to serious health complications and even death.

Inadequate care like not changing diapers properly or frequently enough has a direct impact on health and safety outcomes for nursing home residents. It is, for certain, one of the things I investigate when I learn an elderly nursing home resident suffered a pressure wound.
Consequences When Diapers Are Not Changed
Complications & consequences come up frequently when a nursing home does not do its job properly for residents.
When a diaper is not changed in the proper manner, many health conditions can arise. This includes:
◊ cellulitis
◊ bed sores
◊ boils
◊ rashes
◊ skin deterioration
These conditions can degrade quality of life and in some cases even shorten life. They should be monitored closely by nursing, and by family members who want to make sure nurses and nursing homes are doing their jobs.
Nursing Home Diaper Change Malpractice
This is one of those bad nursing home acts for which filing a lawsuit does not make sense.
The only time that changes is if the inadequate diaper changes caused a serious pressure ulcer injury. If that happened, you need an experienced pressure wound lawyer.
I have investigated and litigated 100+ nursing home pressure wound cases. In fact, the majority of my nursing home cases involve pressure wounds.
Contact me for a free consult on how I can become your advocate. My information is at the bottom of this page.
Warmly,
Reza Davani, Esq.
State Bar No.: #1212110211
Federal Bar No.: #30168
Cellphone: (301) 922-4598
Email: reza@nursinghometruth.com
Pressure Ulcer Legal Library
Click/Tap Icons to Access Articles

Supporting Literature, Citations & Resources:
Al-Samarrai, N. R., Uman, G. C., Al-Samarrai, T., & Alessi, C. A. (2007). Introducing a new incontinence management system for nursing home residents. Journal of the American Medical Directors Association, 8(4), 253–261.
Bitencourt, G. R., Alves, L. D. A. F., & Santana, R. F. (2018). Practice of use of diapers in hospitalized adults and elderly: cross-sectional study. Revista brasileira de enfermagem, 71, 343-349.
Chang, Y. P., Schneider, J. K., & Sessanna, L. (2011). Decisional conflict among Chinese family caregivers regarding nursing home placement of older adults with dementia. Journal of Aging Studies, 25(4), 436-444.
Malmedal, W., Ingebrigtsen, O., & Saveman, B. I. (2009). Inadequate care in Norwegian nursing homes–as reported by nursing staff. Scandinavian journal of caring sciences, 23(2), 231-242.
Svanström, R., Sundler, A. J., Berglund, M., & Westin, L. (2013). Suffering caused by care—elderly patients’ experiences in community care. International journal of qualitative studies on health and well-being, 8(1), 20603.
Ho, C. S., Wong, S. Y., Chiu, M. M., & Ho, R. C. (2017). Global prevalence of elder abuse: A metaanalysis and meta-regression. East Asian archives of psychiatry, 27(2), 43-55.
Prang, I. W., & Jelsness-Jørgensen, L. P. (2014). Should I report? A qualitative study of barriers to incident reporting among nurses working in nursing homes. Geriatric Nursing, 35(6), 441-447.
About the Author
This nursing home and medical malpractice article was written by Baltimore, Maryland nursing home attorney Reza Davani, Esquire. Mr. Davani received his Juris Doctor degree from a Tier 1 law school, the University of Maryland Francs King Carey School of Law. He received his first license to practice law from the State of Maryland’s Court of Appeals (MD State License No. 1212110211), and just four months later received a federal law license from the United States District Court for the District of Maryland (Federal License No. 30168).
Mr. Davani has been practicing law for over 10 years. He began practicing law by helping clients as a sanctioned student lawyer before receiving his law license, and second chaired his first jury trial in federal court before even graduating law school. He is a registered member of the Maryland Association for Justice (MAJ), the American Bar Association (ABA), the American Association for Justice (AAJ), and was formerly on the MAJ’s Legislative Leader’s Circle.
Mr. Davani has taken over 20 cases to trial in state and federal court, and favorably settled well over 100 cases for injured victims. He has personally helped his clients recover over $25,000,000 in personal injury, medical malpractice, and nursing home abuse settlements and verdicts in Maryland and other states. He is dedicated to fighting for justice, and welcomes the opportunity to help you.
About the Nurse Consultant
La kesha Dillard, started her nursing career in 1994 as a Home Health Aide (HHA). She enjoyed working with people so much that she earned her certification as a Certified Nursing Assistant (CNA). She attended Trocaire College and completed both (the LPN and RN) programs where she earned her LPN/RN AAS degree. She was motivated to further her education and in 2016 she received her baccalaureate degree in nursing from Daemen College Amherst, NY. In 2019 she successfully completed Chamberlain College of Nursing, Nurse Executive and Leadership program, and earned a Masters of Science in Nursing (MSN) degree.
Mrs. Dillard wanted to learn more about the business side of nursing, so she attended Devry University and received her Master of Business Administration (MBA) degree in 2023.
In 2021, she successfully completed the Vicky Millazo program where she earned her certification as a Legal Nurse consultant. She opened up her nurse consulting business in 2022 and is the proud owner, founder/CEO at Mrs. RN Consulting, LLC. La kesha has consulted and worked with many attorneys by helping them understand the medical records to get justice for their clients. She has worked at several Long-Term Care facilities (LTC), medical surge units and has several years of experience with patient care and consulting.
She is a strong advocate for patients and believes in Person-Centered Care (PCC) at all times. La kesha is also a tough upholder for staff rights, and she continues to motivate nurse entrepreneurs to further their education in nursing.
Nursing Home Abuse Lawyer Near You in Baltimore, Maryland & Beyond
I can help you anywhere in Maryland, including Allegany County, Anne Arundel County, Baltimore City, Baltimore County, Carroll County, Calvert County, Caroline County, Cecil County, Charles County, Dorchester County, Frederick County, Garrett County, Harford County, Howard County, Kent County, Montgomery County, Prince George’s County, Queen Anne’s County, Somerset County, St. Mary’s County, Talbot County, Washington County, Wicomico County, and Worcester County.
I have helped clients in over a dozen jurisdictions, including California, Delaware, District of Columbia, Georgia, Illinois, Iowa, Massachusetts, Maryland, Mississippi, New Jersey, New Mexico, New York, North Carolina, Pennsylvania, South Carolina, Washington, and Virginia.
I help injured victims nationwide in all 50 states on a case-by-case basis via Pro Hac Vice.